
What Is Chlamydia Trachomatis?
Learn the signs of chlamydia, from discharge and odor changes to common symptoms. Find out when to get tested and how to protect your health.
Words by Olivia Cassano
Scientifically edited by Dr. Krystal Thomas-White, PhD
Medically reviewed by Dr. Kate Stewart, MD
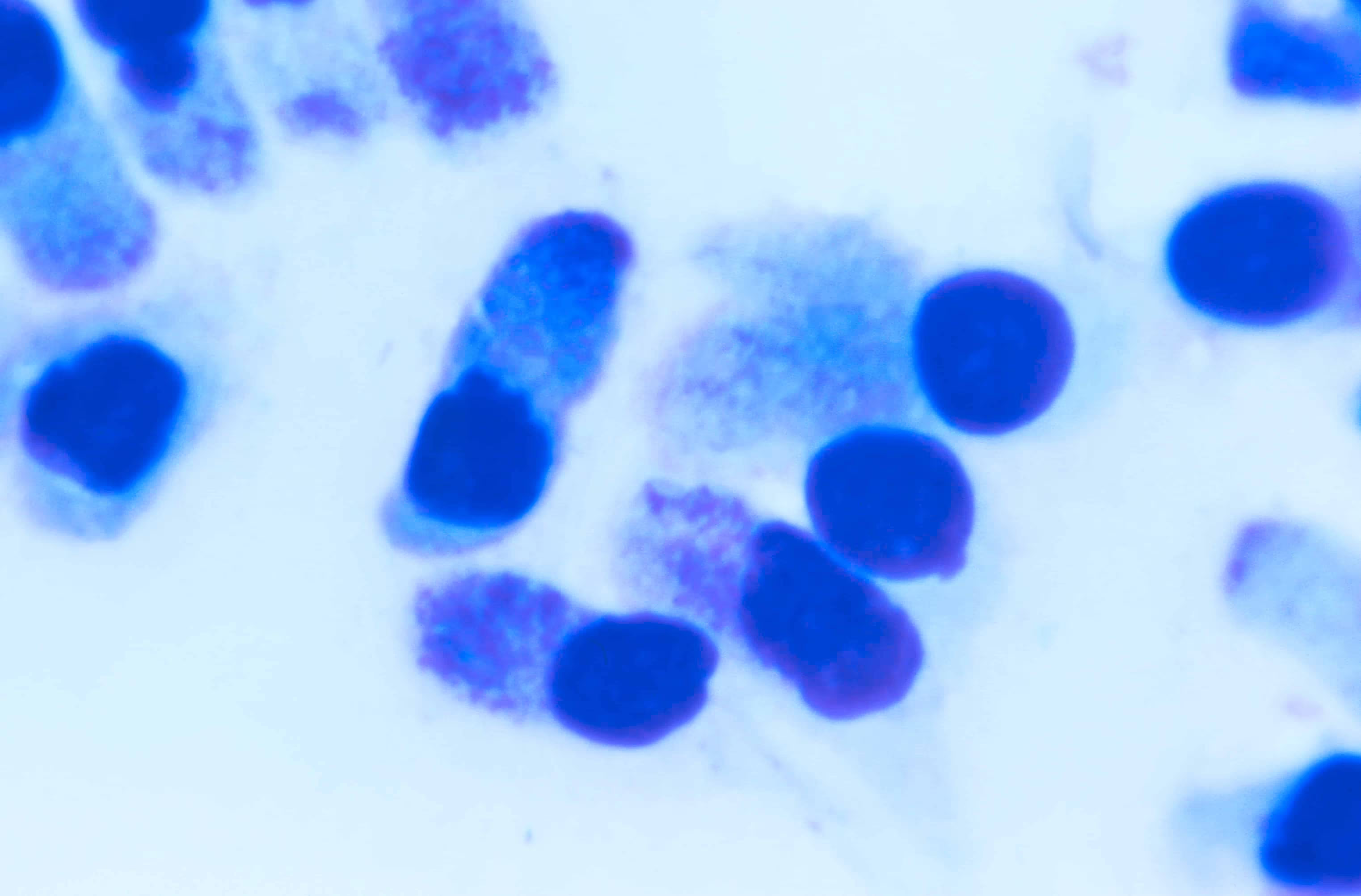
Chlamydia trachomatis (C. trachomatis) is a bacterium that can cause many infections, most notably the sneaky but super common sexually transmitted infection (STI) chlamydia.
Chlamydia is the most common sexually transmitted infection (STI) in the U.S. and worldwide, and it’s estimated that one in 20 sexually active women aged 14-24 years has it.
Sometimes, it can be tricky to spot chlamydia since it may not show any signs, particularly in women. Studies have found that around 80% of women who have the infection aren't even aware of it. Untreated chlamydia can cause some serious health problems, like infertility, ectopic pregnancy, and pelvic inflammatory disease (PID).
Fortunately, chlamydia can be treated effectively with proper diagnosis. So, to stay on the safe side, the key is prevention and regular STI testing. Keep reading to learn more about how to protect yourself from chlamydia and how to treat it.
Symptoms of chlamydia
Chlamydia is often called a "silent" infection because many people don't experience any symptoms and therefore don't know they have it. Unfortunately, this can lead to unknowingly spreading the infection to others.
If you do have symptoms of chlamydia, they can be similar to the symptoms of cervicitis (inflammation of the cervix) or a urinary tract infection (UTI).
Signs of chlamydia in women and people with vaginas include:
- Unusual vaginal discharge that is white, yellow, and has a foul smell
- Pus in your urine (pyuria)
- A frequent need to pee
- A burning sensation when you pee
- Painful sex (dyspareunia)
- Pain or tenderness in the lower belly
- Vaginal bleeding between periods
- Painful periods
- Itching or burning in and around your vagina.
Remember that many of these symptoms can be a sign of other sexually transmitted infections or genital infections. It’s important to speak to your healthcare provider to get a proper diagnosis.

What does chlamydia look like?
Chlamydia can cause yellow, white, thick, or milky discharge with a strong, unpleasant odor. However, everyone's discharge can look different, so it's important to watch for any drastic changes in the color, texture, or smell of your vaginal discharge. Other visible symptoms of chlamydia include cloudy urine and vaginal bleeding or spotting after sex.
Sometimes, chlamydia discharge can be tough to spot because the changes are subtle, and it can be mistaken for other vaginal infections like bacterial vaginosis (BV) or a yeast infection. That's why regular STI testing is crucial. By staying on top of your vaginal health, you can catch any potential issues early and get the needed treatment.
What does chlamydia discharge smell like?
The smell of chlamydia discharge can be subtle or even absent. However, when it’s present, it’s often described as:
- Foul or unpleasant
- Fishy or musty
- Sharp or pungent.
It's important to note that chlamydia discharge doesn’t always have a distinct smell. A foul odor may not automatically mean chlamydia, as other infections or conditions can also cause smelly vaginal discharge. If you notice an unpleasant odor, it’s a good idea to see a healthcare provider for an accurate diagnosis.
How long does it take for chlamydia to show up?
It's not always easy to know when chlamydia symptoms will show up since Chlamydia trachomatis takes a while to reproduce and cause an infection. It can take a few weeks after exposure before symptoms occur, but it might take as long as a couple of months. You should wait at least two weeks after having unprotected sex before getting tested.
If you're sexually active, getting tested for sexually transmitted infections regularly is important, even if you feel fine. You could have a chlamydia infection and pass it to others without realizing it, so it's best to be safe and get tested. So, don’t wait for symptoms to show up!

Recurrent symptoms? Get Evvy's at-home vaginal microbiome test, designed by leading OB-GYNs.
What causes chlamydia
Chlamydia is spread through unprotected vaginal, anal, or oral sex with someone who has the infection. You can also contract chlamydia by sharing sex toys with someone with the condition. That's because the bacteria that causes chlamydia (Chlamydia trachomatis) can be transferred through vaginal fluid and semen.
It can be challenging to know if a current or potential partner has chlamydia because many people with the infection do not experience symptoms. To prevent chlamydia, it's important to practice safe sex and always:
- Use condoms during penetrative vaginal or anal sex
- Use dental dams or condoms during oral sex
- Use dental dams during vagina-to-vagina contact
- Wash sex toys or cover them with a clean condom before sharing them with a sexual partner
- Get tested for STIs regularly, especially if you have multiple sexual partners.
It is also important for pregnant women to get tested for chlamydia. Women who have chlamydia can pass it on to their baby during childbirth, and this can cause eye or lung infections in the newborn.
Can you get chlamydia from oral sex?
Yes, a Chlamydia trachomatis infection can be transmitted to the throat through oral sex. Oral chlamydia isn't as common as genital chlamydia, but it's still important to be aware of it. People with oral chlamydia often don't experience any symptoms, or they might just have a sore throat. You can prevent oral chlamydia by using a condom or a dental dam during oral sex.
How to treat chlamydia
If you're diagnosed with chlamydia, you can quickly treat the infection with antibiotics. The most commonly prescribed antibiotics for chlamydia are doxycycline, which is taken for seven days, and azithromycin, which is usually taken as a single dose (and is the recommended option if you're pregnant).
It's important to follow your healthcare provider's instructions when taking antibiotics and complete the entire course of medication, even if you start feeling better or your symptoms disappear.
When it comes to chlamydia, prevention is key, so it's a smart idea to include a chlamydia test as part of your regular health routine, especially for women, who are at higher risk of contracting chlamydia.
The Centers for Disease Control and Prevention (CDC) recommends yearly chlamydia screening for all sexually active women younger than 25 or at higher risk of contracting chlamydia. Risk factors for chlamydia include:
- Being under 25
- Being pregnant
- Having sex with a new partner
- Having multiple sexual partners
- Having had a chlamydia infection in the past.
The CDC also recommends testing for chlamydia if you’re getting an intrauterine device (IUD) fitted. If left untreated, chlamydia infections can be transferred from the vagina into the uterus by the insertion of an IUD, which could lead to PID.
How is chlamydia diagnosed?
To diagnose chlamydia, your healthcare provider may recommend something called a nucleic acid amplification test (NAAT). This involves providing a fluid sample through a vaginal/cervical swab or, less commonly, a first-catch urine sample (but urine may detect 10% fewer infections than vaginal/cervical swabs). The sample is then sent to a lab to see if Chlamydia trachomatis is present.
You can also choose to do an at-home chlamydia test, like with Evvy's Vaginal Health Test and Expanded PCR Panel, by doing a vaginal swab and sending the sample to a lab.
Chlamydia might not show up in test results right away. Sometimes, it can take up to two weeks for Chlamydia trachomatis to be detected. So, to get the most accurate results, it's best to wait at least 14 days after sexual contact before getting tested.
Can chlamydia go away on its own?
You shouldn't ignore chlamydia or wait for it to go away on its own. An untreated infection can lead to some serious health problems, such as:
- Pelvic inflammatory disease (PID), an inflammation of the upper genital tract
- Formation of scar tissue that blocks the fallopian tubes
- Infertility
- Ectopic pregnancy
- Chronic pelvic pain.
In rare cases, untreated chlamydia can also spread to your bloodstream and put you at a higher risk of reactive arthritis (chronic inflammation of the joints) and human immunodeficiency virus (HIV).
How long does it take for chlamydia to go away?
With treatment, chlamydia will go away within a week or two. But it's essential to get another chlamydia test three months after the treatment to make sure you're all better.
If you've been given a single dose of antibiotics, it's best to avoid having sex for about seven days. If you're taking a seven-day course of antibiotics, you shouldn't have sex until you finish the treatment and all your symptoms go away. This is to stop the infection from spreading to your partner(s).
Any recent sexual partners should also be treated for chlamydia at the same time. Luckily, most states offer something called Expedited Partner Therapy (EPT), so any sex partner can receive chlamydia treatment without needing to be examined by a healthcare provider first.
Can chlamydia come back?
Unfortunately, repeat infection with chlamydia is pretty common. You’re at higher risk of contracting chlamydia if you’ve had it in the past. The infection might also come back if you didn’t finish your course of antibiotics or if your partner(s) weren’t treated for chlamydia.
FAQ
What does Chlamydia trachomatis cause?
Chlamydia trachomatis is the bacterium that causes the sexually transmitted infection chlamydia.
How can you get Chlamydia trachomatis?
You get a chlamydia infection by having unprotected vaginal, anal, and oral sex with someone who has the infection. Since Chlamydia trachomatis is spread through vaginal fluid and semen, it’s also possible to get chlamydia by sharing sex toys with someone who has the infection.
Does Chlamydia trachomatis go away?
Yes, chlamydia can be treated and cured with antibiotics (most commonly doxycycline or azithromycin). The infection should go away in just one or two weeks with treatment. We know it can feel really embarrassing to get a sexually transmitted infection, but you should never ignore it or wait for it to go away on its own.
Is chlamydia the same as gonorrhea?
No, chlamydia and gonorrhea are two different sexually transmitted infections. Although they're both incredibly common and can cause similar symptoms, chlamydia is caused by the bacterium Chlamydia trachomatis, while gonorrhea is caused by the bacterium Neisseria gonorrhoeae.
How serious is Chlamydia trachomatis?
All sexually transmitted infections can have serious consequences if left untreated. For women and AFAB people, chlamydia can lead to pelvic inflammatory disease, chronic pelvic pain, ectopic pregnancy, and infertility. An untreated Chlamydia trachomatis infection can also put you at higher risk of developing reactive arthritis and contracting other STIs, including an HIV infection. It's crucial to seek medical attention if you suspect you may have contracted a chlamydia infection, and make both safe sex practices and routine STI testing a habit.
Can chlamydia cause itching?
Yes, chlamydia can cause itching in women, although it's not the most common symptom. Many women with chlamydia don’t notice any symptoms at all, which is why it’s often called a “silent” infection. When symptoms do appear, they can include abnormal vaginal discharge, a burning sensation when you pee or have sex, pelvic pain, and sometimes itching or irritation in the vaginal area. The itching is usually due to inflammation or irritation of the vaginal or cervical tissues caused by the infection. However, because itching is also common with other conditions like yeast infections or bacterial vaginosis, it’s important not to self-diagnose. If you're experiencing vaginal itching — especially along with other symptoms like discharge or discomfort — it's a good idea to see a healthcare provider for proper testing and treatment.





