
Mycoplasma Genitalium: Symptoms & Treatment
What is mycoplasma genitalium? Understand the symptoms, mycoplasma genitalium testing, treatment options for this STI, and how to manage it effectively.
Words by Olivia Cassano
Scientifically edited by Dr. Krystal Thomas-White, PhD
Medically reviewed by Dr. Kate Stewart, MD
Mycoplasma genitalium, also called Mgen or M. genitalium, is a sexually transmitted bacteria. And as far as sexually transmitted infections (STIs) go, it’s the new kid on the block — so you may have never heard of it.
STIs like chlamydia, gonorrhea, and HIV can have serious consequences if left untreated. Chlamydia, for example, can lead to infertility, and gonorrhea is becoming increasingly resistant to antibiotics. An HIV infection can lead to AIDS, and even human papillomavirus (HPV), can increase your risk of cervical cancer. But when it comes to Mycoplasma genitalium, there's fairly limited data, so there's still a lot we don't know.
Although it’s not a very common sexually transmitted infection (only 0-5% of women have it), some experts are concerned that Mycoplasma genitalium could become the "new superbug" due to drug resistance — meaning the medications we have available might not work to treat it. Therefore, it is important to be aware of its existence.
Below is what we currently know about Mycoplasma genitalium, including symptoms, treatment options, and how it can affect your sexual health.
What is Mycoplasma genitalium?
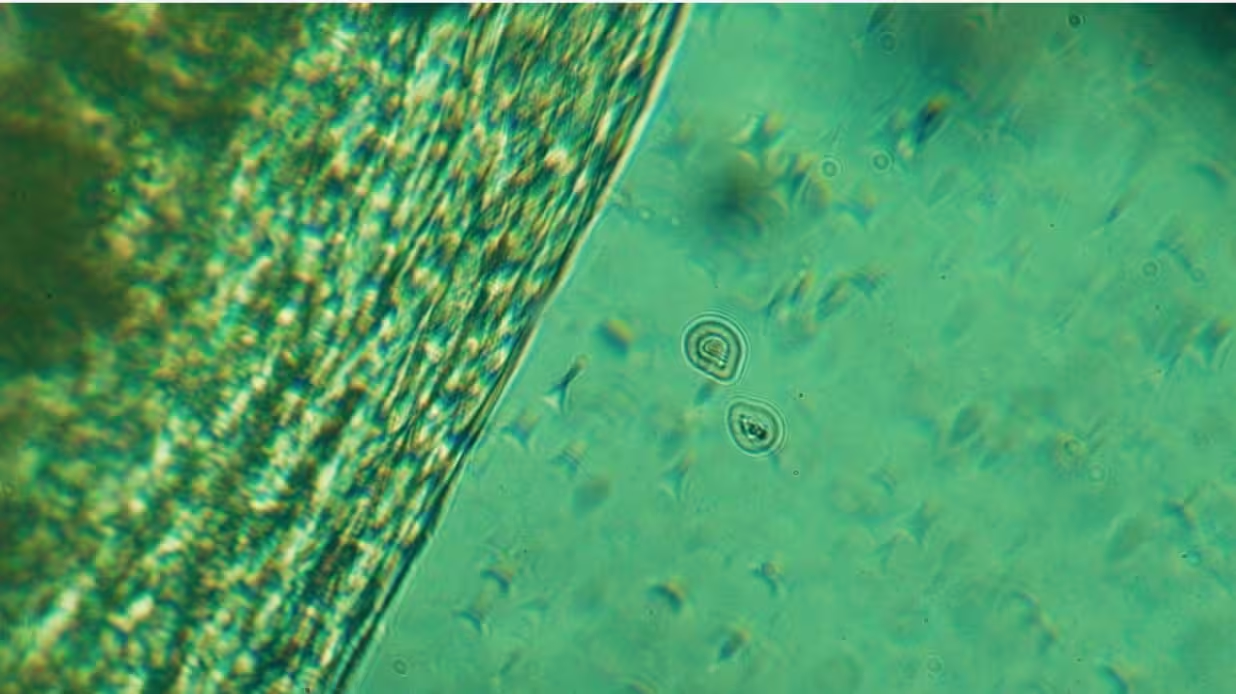
Mycoplasma genitalium belongs to the Mollicutes class, which are different from other bacteria because they don't have a cell wall.
Mycoplasma genitalium is the tiniest bacteria of this kind and is notoriously difficult to cultivate and study in the laboratory, partly why there's so much we don't know about it.
Mycoplasma genitalium was first identified in the early 1980s but mostly went unnoticed until 2015 when a study in the Journal of Epidemiology linked it to sexual activity. It’s the only Mycoplasma species recognized by the Centers for Disease Control and Prevention (CDC) as an STI.
Mycoplasma genitalium can live in your reproductive tract — including your vagina, uterus, fallopian tubes, and urethra — without causing any problems. However, if the bacteria begin to multiply and take over, they can cause an infection.
A meta-analysis found that Mycoplasma genitalium is linked to various conditions in women, such as:
- cervicitis (inflammation of the cervix)
- pelvic inflammatory disease (PID)
- infertility
- preterm birth
- ectopic pregnancy.

Recurrent symptoms? Get Evvy's at-home vaginal microbiome test, designed by leading OB-GYNs.
How do you get Mycoplasma genitalium?
Like all sexually transmitted infections, you can contract Mycoplasma genitalium through sexual contact, such as unprotected:
- vaginal sex
- oral sex
- anal sex.
Although it's less likely, Mycoplasma genitalium can also be spread by sharing sex toys.
Mycoplasma genitalium can affect anyone sexually active, regardless of gender or sexual orientation, so condom use — or other barrier methods of birth control, such as dental dams — is the best way to prevent it.
Mycoplasma genitalium symptoms
A Mycoplasma genitalium infection is often asymptomatic, and many people don't know they have it. When symptoms do show up, they're really similar to those of other sexually transmitted infections such as chlamydia and gonorrhea.
Common Mycoplasma genitalium symptoms include:
- Unusual discharge
- Pelvic pain
- Itching in and around the vagina
- Bleeding between periods and/or after sex
- Pain during sex or while peeing.
As mentioned above, these symptoms can be caused by other infections. Getting tested and speaking to your healthcare provider if you notice any of these symptoms is a good idea.
How to test for Mycoplasma genitalium
To diagnose Mycoplasma genitalium, your healthcare provider may recommend Mycoplasma genitalium testing, typically done through a nucleic acid amplification test (NAAT).
This involves providing a fluid sample through a vaginal/cervical swab or, less commonly, a urine sample. The sample is then sent to a lab to see if Mycoplasma genitalium is present. You can also do an at-home STI test, such as Evvy's Vaginal Health Test and Expanded PCR Panel, to see if you have Mycoplasma genitalium.
The CDC advises that people who aren't showing symptoms don't need routine Mycoplasma genitalium testing. However, if you or your sexual partners have signs of Mycoplasma genitalium infection, you should get tested.
The CDC also recommends testing for Mycoplasma genitalium if you took treatment for urethritis and cervicitis, but the infection didn’t go away.
Mycoplasma genitalium treatment
Mycoplasma genitalium can be treated with antibiotics. In the past, the preferred treatment was a single dose of the antibiotic azithromycin. But, recent studies have shown that this type of bacteria has become resistant to azithromycin, making it ineffective.
Now, doctors test patients for Mycoplasma genitalium bacteria to see if it has mutated into a variant resistant to azithromycin. If it hasn't developed drug resistance, the recommended antibiotic treatment is doxycycline and azithromycin. If it has developed macrolide resistance, doctors recommend doxycycline and moxifloxacin.
FAQ
Is Mycoplasma genitalium always an STD?
Yes, Mycoplasma genitalium is a type of bacterial infection that is spread via unprotected sex. Although it’s been around for a while, it was only classified as a sexually transmitted disease by the CDC in 2015. It’s the only Mycoplasma species considered a sexually transmitted infection.
How do I test for Mycoplasma?
Testing for Mycoplasma, including Mycoplasma genitalium, typically involves collecting a swab from the vagina or cervix. The sample is analyzed using nucleic acid amplification tests (NAATs), which detect the bacteria's genetic material with high accuracy. Evvy’s Vaginal Health Test Expanded PCR Panel uses advanced metagenomic sequencing to analyze the vaginal microbiome and can detect Mycoplasma genitalium along with other microbes. By identifying the presence and relative abundance of this pathogen, you get a detailed insight into the bacterial composition and potential imbalances that may be contributing to symptoms or conditions.
Does a pap smear test for Mycoplasma?
No, a Pap smear doesn't check for Mycoplasma. It's actually a test that screens for any changes in cervical cells, especially those caused by human papillomavirus (HPV), which can potentially lead to cervical cancer. During a Pap smear, cells from the cervix are collected and examined under a microscope to look for any precancerous or cancerous changes. If you’re looking to test for Mycoplasma genitalium or other Mycoplasma types, those require specific tests, like nucleic acid amplification tests (NAATs), which aren’t included in a standard Pap smear.
Does Mycoplasma genitalium go away?
Yes, Mycoplasma genitalium is totally curable with adequate treatment. The infection can be treated with antibiotics. That said, research shows that drug resistance is becoming more and more prevalent with M. genitalium infections, so there's a high prevalence of treatment failure.
Does Mycoplasma mean cheating?
If you or your partner test positive for Mycoplasma genitalium (or another sexually transmitted infection), it doesn't necessarily mean that anyone cheated. There are a few things to keep in mind. Many STIs, like Mycoplasma genitalium, can stay dormant for months or even years without causing any symptoms. This means that a person could have gotten the infection from a previous relationship and only recently started showing symptoms or got tested. Keep in mind that many people with Mycoplasma genitalium don't have any symptoms and could unknowingly pass on the infection. It's also possible that the infection was from a previous partner and went undetected.
Is Mycoplasma genitalium the same as chlamydia?
No. Mycoplasma genitalium and chlamydia are two different sexually transmitted infections, although they have similar symptoms and can both lead to complications like pelvic inflammatory disease. The good news is that they can both be treated, but it's important to get tested so you can receive the appropriate treatment.
What are the signs and symptoms of Mycoplasma genitalium?
Mycoplasma genitalium is often asymptomatic (meaning it doesn’t cause any symptoms). When it does cause symptoms, however, some common ones in women are unusual vaginal discharge, a burning sensation when you pee, pain during sex, and bleeding in between periods or after sex.





