Can My IUD Cause Bacterial Vaginosis or a Yeast Infection?
Are IUDs an effective birth control method, and do they impact the vaginal microbiome or increase the risk of infections like BV or yeast infections?
Scientifically edited by Dr. Krystal Thomas-White, PhD
Medically reviewed by Dr. Christine Vo, MD
If you’ve ever experienced the misfortune of forgetting to pick up your hormonal birth control pills from the pharmacy, you’ll likely appreciate why intrauterine devices (IUDs) are beloved by many. First of all, they’re low-maintenance since they only require one appointment at the gynecologist every few years for insertion. Once they’re in, they’re basically mistake-proof, making them extremely effective (over 99%) in preventing pregnancy. And if you change your mind about wanting to get pregnant (or just don’t want an IUD anymore) they’re also easily removable.
But as most of us know all too well, in the world of vaginal health, there are sadly no free passes. Despite the IUD being a great option for birth control, you may have heard that IUDs can cause other problems, like increasing your risk of bacterial vaginosis (BV) and yeast infections.
But can an IUD cause BV or other vaginal infections? And if so, do the risks outweigh the benefits compared to other birth control methods? Below, we cover existing research on the relationship between vaginal infections and IUDs, so you have all of the info you need to make the best birth control decision for you.
What is an IUD?
An IUD is a form of long-acting reversible contraception (LARC). To insert, a medical professional dilates your cervix and places the IUD in your uterus.
In addition to preventing pregnancy, IUDs are also prescribed by doctors as a treatment for very heavy bleeding during your period, painful periods (dysmenorrhea), pelvic pain/endometriosis, and endometrial hyperplasia/endometrial cancer.
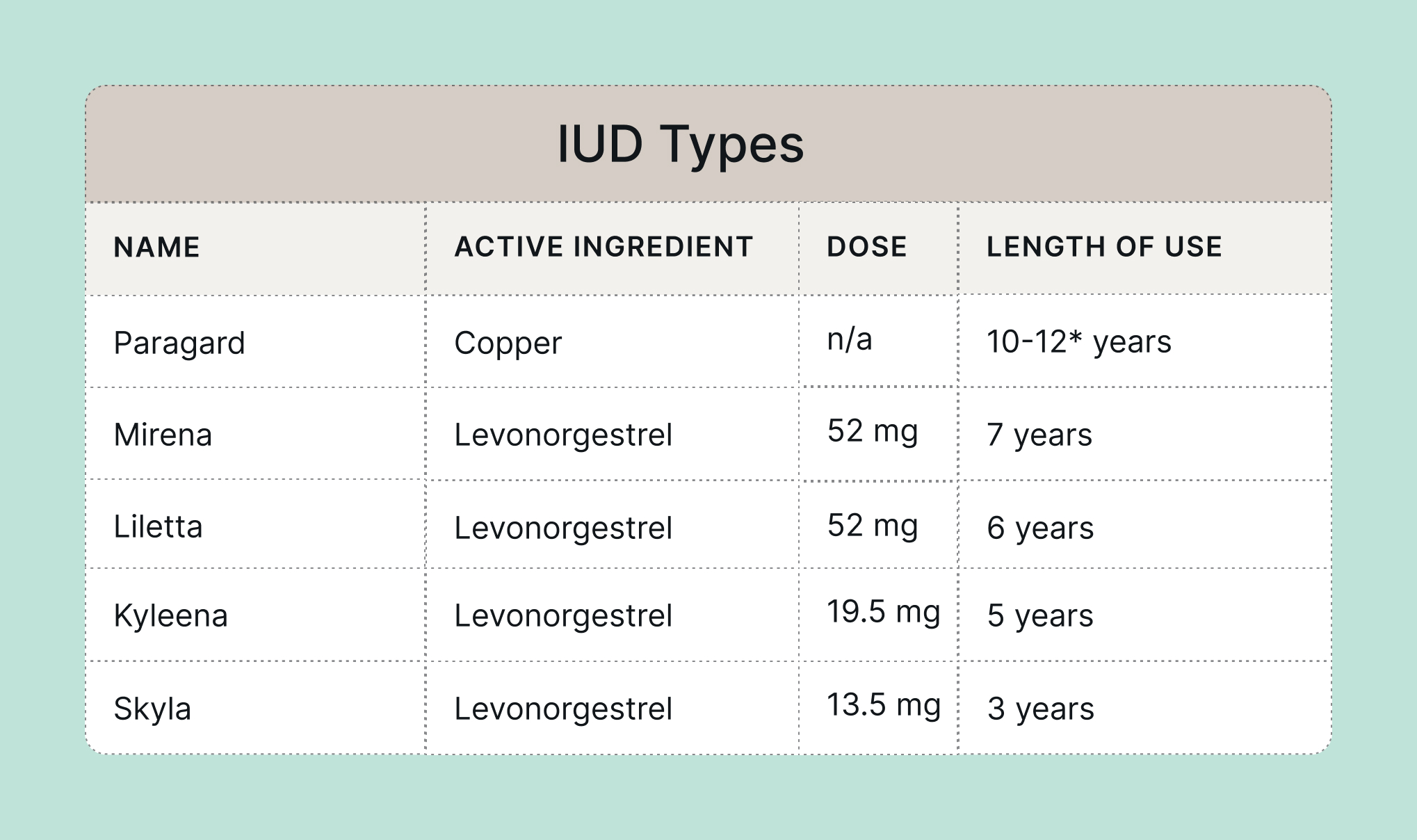
Currently, there are five available IUDs on the market in the U.S. Of women in the U.S. who use IUDs, three-quarters use a hormonal one, and about one-quarter use copper. (Another use for the copper IUD is as emergency contraception for up to five days after unprotected sex.)
Here are some quick stats on the five types:
Non-hormonal IUDs and vaginal infections
Here’s the short (and frustrating) answer: copper IUDs may influence microbes in the vagina, but we need more data since the evidence is mixed.
Ok, but what does that mean for my vagina? Some women with copper IUDs may have a higher prevalence of Candida (yeast), as well as higher rates of bacterial vaginosis.
A 2014 study examined 108 women who received a copper IUD and found that after 12 months, they had a slightly higher prevalence of Candida species, Mycoplasma, and signs of inflammation than they did before getting their IUD. Another study that assessed a copper IUD used by 95 women in Iran found that there was a higher prevalence of Candida in vaginal samples three months after insertion. But, since these studies had a limited number of participants, more research is needed to say for sure if copper IUDs are associated with an increased risk of yeast infection.
Researchers have also studied whether copper IUDs shift the makeup of the vaginal microbiome (and lead to vaginal dysbiosis) as some vaginal infections aren’t caused by a single microbe (we’re looking at you, bacterial vaginosis).
One 2018 study of women in Thailand found no difference in the rate of bacterial vaginosis between women with and without a copper IUD. However, a 2020 study showed that bacterial vaginosis occurred more frequently in participants with copper IUDs than in participants with a hormonal IUD or not using contraception. Additionally, another 2021 study conducted in Africa found that women with copper IUDs had a slightly increased risk of bacterial vaginosis compared to women without IUDs.
Non-hormonal IUDs and STI transmission
Another question that often comes up is whether copper IUDs increase your risk for a sexually transmitted infection (STI). Before we go into that relationship, remember that the pathogens that cause STIs are sexually transmitted and do not come from the IUD itself.
That said, in a 2019 study that compared the rates of sexually transmitted infections across women using different methods of contraception, women with copper IUDs had an increased rate of Trichomonas vaginalis infections, but not other types of STIs such as chlamydia and gonorrhea.
Researchers believe that susceptibility to a Trichomonas infection might be influenced by the microbiome. Meaning, since there’s some evidence to suggest that copper IUDs are related to a higher chance of developing bacterial vaginosis, this disruption to the microbiome might also pave the way for Trichomonas infections, as bacterial vaginosis can increase your risk for STIs. However, more research is needed to confirm if changes to the microbiome are a result of the Trichomonas infection or part of their cause (basically a “chicken or the egg” question).
Hormonal IUDs and vaginal infections
There is even less data on hormonal IUDs and their impact on the vaginal microbes compared to copper IUDs. Why? Hormonal IUDs are newer, and mainly available in the U.S. and Europe. Copper IUDs have been around longer, and are used more widely around the world, so there are more opportunities for researchers to collect data on them.
Do hormonal IUDs cause yeast infections?
TL;DR: it looks like that over a longer period (say, several years), there could be an association between hormonal IUDs and an increased chance for yeast infection. However, it’s unclear why — so back to the lab!
There isn’t a clear verdict on whether or not hormonal IUDs are associated with yeast infections. On the one hand, a report of three different types of studies all conclude that hormonal IUDs are not associated with an increased risk of yeast infections. Also, the same 2014 study that looked at copper IUDs also took a look at 42 women with hormonal IUDs, again looking for Candida species, Mycoplasma, and signs of inflammation. Unlike copper IUDs, the cohort of women receiving a hormonal IUD did not have an increase in any of the three markers of infection one year after insertion.
That said, another study of women who received their IUDs in 1998 looked across seven years after IUD insertion and saw that the chance of having yeast present in a vaginal sample is increased during years 4-7 compared to the first year.
A more recent study looked at the microbes present over five years after hormonal IUD insertion and also found an increase in Candida over time compared to before insertion. Additionally, one recent study from 2020 found that participants with a hormonal IUD did have an increased chance of having a yeast infection two years after their IUD was placed, compared to a copper IUD and a control group without contraception.
Do hormonal IUDs cause bacterial vaginosis?
As far as hormonal IUDs’ associations with other shake-ups to the microbiome: one 2014 study looked at vaginal microbiomes one week before and 12 weeks after hormonal IUD placement and found that the vaginal microbiome changed very little for the 11 participants in the study.
However, a more recent study with 252 women who all got the Mirena IUD looked at a longer time course for changes in the vaginal microbiome and saw a temporary decrease in Lactobacillus and an increased chance of bacterial vaginosis for participants at three months post-insertion. But, that trend was reversed at both one and five years post-insertion, meaning the microbiome was able to return to its pre-insertion state.
IUDs and pelvic inflammatory disease
If you’ve Googled “IUD” and “infection” you may have come across pelvic inflammatory disease (PID). PID refers to an infection in your upper genital tract, such as in the uterus or fallopian tubes. While it’s possible for an infection causing PID to have started out in the vagina, PID is considered a separate condition from a vaginal infection.
If your IUD is being placed by a trained medical professional (which it should be), the chance of vaginal microbes moving into the uterus during the insertion process is very low. One 2012 study of over 57,000 IUD insertions in northern California found that the overall risk for PID after IUD insertion was 0.54%. If you are considering getting an IUD and are worried about your chances of PID, definitely talk to your OB-GYN about your options and whether or not you could have any risk factors for PID.

Recurrent symptoms? Get Evvy's at-home vaginal microbiome test, designed by leading OB-GYNs.
I’m thinking about getting an IUD but I’m worried about vaginal infections
Though having an IUD usually means you can adopt a “set it and forget it” attitude about birth control, getting one can feel like a big decision for many people, especially those who experience recurrent vaginal infections.
We know that all of this mixed evidence on IUDs and their relationship to bacterial vaginosis and yeast can be frustrating. We need more studies on the effects of IUDs on the vaginal microbiome, especially given their increasing popularity. IUD usage in the U.S. has been on the rise since the 1990s. Copper IUDs are also used widely across the globe. More types of copper IUDs, in addition to Paragard, are also expected to be approved in the U.S. soon.
While researchers keep working on these important questions, here are a few things you can do if you’re thinking about getting an IUD and have had your fair share of pesky vaginal infections!:
- Talk to your doctor about your overall risk factors, and discuss what preventative measures you can take before getting your IUD inserted.
- Take an Evvy test before getting your IUD inserted. This can help you to track any changes after insertion because you can test overtime with Evvy (and in case you were wondering, yes, you can swab your vaginal microbiome with an IUD inserted).
- Consider the pros and cons of different types of IUDs for your body.
- If an IUD isn’t the right choice for you, consider other long-acting reversible contraceptive methods, such as Nexplanon, the birth control implant that goes in your arm.
For what it’s worth, you deserve a reliable birth control method that doesn’t mess with your vaginal microbiome or cause you undue anxiety. Team Evvy is here to support your journey in finding a birth control method that works for you so you can feel in control of your body and reproductive health.
FAQ
Does removing IUD help BV?
Some research suggests that IUDs can temporarily increase your risk of bacterial vaginosis, but there isn’t enough data to know for sure if there’s a causational link between the two. That said, if you’ve had recurrent bacterial vaginosis (which doesn’t respond to treatment), and you have an IUD fitted, removing the device could be a solution. Please speak to your healthcare provider if you’re thinking of removing your IUD.
Can IUD mess up your pH balance?
Some studies found that IUDs (both hormonal and non-hormonal) can cause a temporary shift in the vaginal microbiome for some women. The reality is that we need more studies on the effects of IUDs on the vaginal microbiome. It’s also worth pointing out that your pH balance is influenced by a lot of factors. For example, sex itself is more likely to affect your vaginal pH — especially unprotected sex, or sex with multiple sexual partners. If you’re thinking about getting an IUD but are worried about vaginal infections, speak to your healthcare provider about your overall risk factors, and discuss other potential birth control options.
Can IUD cause yeast infections?
Some studies have shown that IUD users have higher levels of Candida strains than women without IUDs — but the evidence is mixed. Data shows that the risk might be higher if you have a non-hormonal (copper) IUD, while there isn’t a clear verdict on whether or not hormonal IUDs are associated with yeast infections. Frustrating, we know!