What Is a Yeast Infection? The Ultimate Guide
What is a vaginal yeast infection? Discover symptoms, diagnosis, and treatment in our ultimate guide to yeast infections.
Words by Monica Karpinski
Scientifically edited by Dana Alloy
Medically reviewed by Dr. Sabrina Sahni, MD NCMP
Most people with vaginas have probably heard of yeast infections. They're a super common type of fungal infection and although they're mostly harmless, they can really mess with your vaginal health and everyday life. But what is a yeast infection caused by? And more importantly, how do you treat it? Keep scrolling to learn more about vaginal yeast infections.
What is a yeast infection?
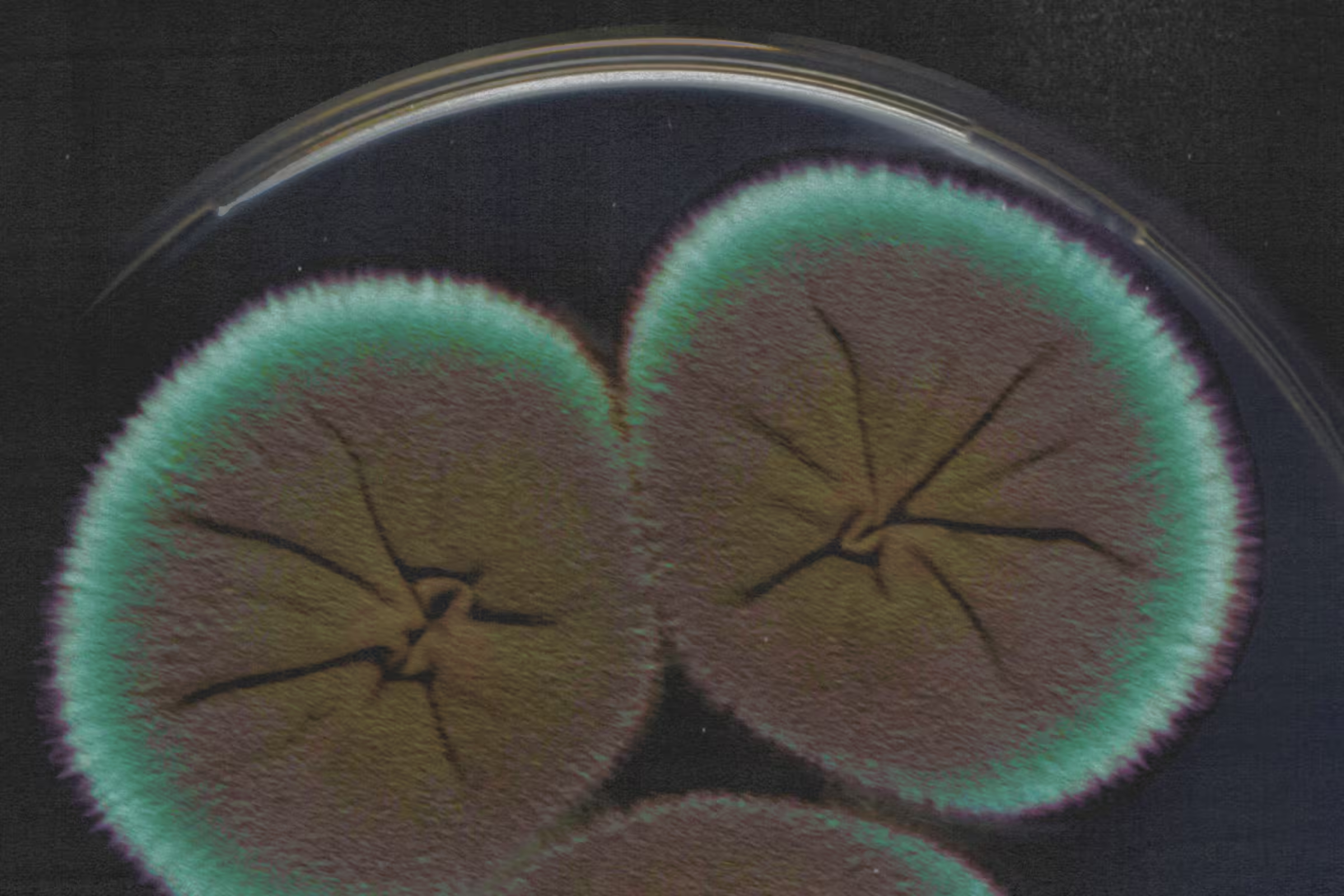
A vaginal yeast infection, also known as vaginal candidiasis, is a common fungal infection caused by an overgrowth of Candida fungi, most commonly Candida albicans.
Candida lives on our skin and in various nooks and crannies within the body, including the mouth, throat, and vagina. Though fair amounts of Candida can be found in the vaginal microbiomes of healthy people, sometimes, Candida can overgrow and become a vaginal yeast infection.
If you’ve had one or think you might have one, you’re far from alone — up to 75% of women will have a vaginal yeast infection at least once in their lifetime.
Vaginal yeast infections can be anything from mild and annoying to severe and recurring. Given their prevalence, it’s important to understand the signs, symptoms, and causes, so that you know how to best care for your body and when to seek treatment.
Yeast infection symptoms
Most people associate a yeast infection with itchiness — a symptom caused by inflammation of the vulva and vagina. However, it can cause other symptoms, too.
The symptoms of a yeast infection may include:
- Vulvar and vaginal itching redness, or soreness
- White vaginal discharge, that is curd-like in consistency and does not often smell
- Pain during sex
- A burning sensation when you pee.
However, these can also be signs of other conditions, so be sure to get checked out by a healthcare provider if you’re actively having symptoms. They’ll be able to provide an accurate diagnosis and tell you if your symptoms are caused by a yeast infection or something else.

Recurrent symptoms? Get Evvy's at-home vaginal microbiome test, designed by leading OB-GYNs.
What does a vaginal yeast infection look like?
Perhaps the most obvious visual sign of a vaginal yeast infection is a change in vaginal discharge. You’ve maybe heard of the “cottage cheese” analogy and true to its comparison, a yeast infection creates discharge that is a whitish-yellow color with a curdish consistency. Another sign of infection can be swelling and soreness of the vulva.
What does a vaginal yeast infection smell like?
One indication that it may not be a yeast infection? A fishy or foul smell.
If yeast infections cause odor, some may notice a yeasty smell, like beer or bread, while others may not notice any smell at all. However, if you notice a foul, rotten, or fishy smell, it may be a different condition, such as bacterial vaginosis (BV), trichomoniasis, or chlamydia. In this case, it's best to seek medical attention as soon as possible.
How is a vaginal yeast infection diagnosed?
If you suspect you have a yeast infection, your doctor will first ask you about your symptoms and medical history. They will then perform a pelvic exam to examine your vulva and vagina for signs of infection, such as swelling, redness, and abnormal discharge. Like many other gynecological exams, doctors may use a speculum to examine the inside of your vagina and cervix.
Your doctor may also take a swab of vaginal fluid from the inside of your vagina, which can be examined under a microscope or in the lab for signs of yeast species. While treating by phone — or even online questionnaire — is becoming increasingly more common, advocating for a vaginal yeast culture as opposed to relying on symptoms alone can help to prevent misdiagnoses and unnecessary antifungal overuse.
Think twice before self-diagnosing a yeast infection
As some types of medication used to treat vaginal yeast infection symptoms are available over the counter, many people also choose to self-diagnose. But self-diagnosing isn’t always reliable, as other vaginal infections can often be mistaken for a yeast infection!
In one study of 601 cisgender women, only around half self-diagnosed their vaginal yeast infection correctly. Another analysis of 153 patients found that 74% were incorrect in diagnosing themselves with a vaginal yeast infection, while in yet another, only 61% of bacterial vaginosis and 77% of vaginal yeast infection diagnoses among 220 people were incorrect. You get the idea!
What’s more, using antifungals or other yeast infection products when you don’t have one may irritate your vulva/vagina or exacerbate conditions like bacterial vaginosis or cytolytic vaginosis.
How to treat vaginal yeast infections
Generally, antifungal medicines are considered the first-line option to treat yeast infections. Your doctor will recommend treatment depending on how severe your infection is and how frequently it recurs, if at all.
If you're experiencing mild or moderate vaginal symptoms that do not frequently recur (also known as an "uncomplicated infection"), your doctor may prescribe a short course of vaginal antifungal medicine in cream, ointment, or suppository form. These medications often end in “-azole,” such as terconazole or miconazole. Alternatively, you may be given a single, oral dose of a medicine called fluconazole. However, fluconazole isn't recommended if you are pregnant.
For more severe or frequent infections, you may need to take multiple oral doses of antifungal medication or be prescribed a longer course of vaginally-inserted antifungal medications.
If the infection isn’t responding to antifungal drugs, then your doctor may recommend other medicines such as boric acid, nystatin, or flucytosine, which can be taken as a vaginal suppository.
What if my vaginal yeast infection doesn’t respond to treatment?
Sometimes, a vaginal yeast infection doesn’t clear up, even when you’re taking medication. If this is you, don’t panic — it could be because that particular medication doesn’t work on the type of yeast that’s causing your infection.
Most yeast infections — up to 90% — are caused by Candida albicans (C. albicans), but other strains can overgrow in the same way. These include Candida glabrata (C. glabrata), responsible for around 5% of cases, plus C. tropicalis, C. parapsilosis, and C. krusei, among others.
You may also experience recurrent yeast infections, which are usually defined as three or more episodes of symptomatic vaginal yeast infections within a year. This affects <5% of women, but can be substantially disruptive to quality of life — if you are experiencing recurrent yeast infections, know that you are not alone.
Treating different strains of Candida
When a yeast infection is caused by a fungus other than C. albicans, it is considered a "complicated yeast infection". In this case, your doctor may recommend different types of treatment, such as a longer or higher-strength dose of medication, or a combination of different medicines.
For instance, the initial antifungal treatment for C. albicans infections might not be as effective for other strains, while certain antifungal treatments may not work well for infections caused by C. glabrata. In such cases, your doctor might suggest using boric acid instead. Additionally, the vaginal cream terconazole is typically recommended for infections caused by yeasts other than C. albicans and C. glabrata.
Taking treatment for the wrong yeast might also explain why your vaginal infection just keeps coming back. It’s always best to check in with your doctor if your yeast infection isn’t responding to treatment. It may be the case that your symptoms are being caused by something else, such as cytolytic vaginosis (CV)— when healthy bacteria overgrow — which can also be itchy and cause vaginal discharge.
What are the risk factors for yeast infections?
There's no surefire way to prevent a yeast infection from happening, and how effective any precautions are can depend on individual factors — including your medical history and sexual behaviors. However, here are some common risk factors, that can cause Candida to overgrow.
Antibiotics
Antibiotics are the most frequent and predictable cause of yeast infections. Various studies have shown that yeast infections are more common in those taking antibiotics, but exact numbers differ depending on the size and location of the study.
Despite a clear association between antibiotics and Candida overgrowth, the reason why is still TBD by further scientific research (yet another question we hope Evvy can help answer!) It’s important to note that all classes of antibiotics — not only antibiotics for vaginal issues — can increase risk.
People who have some Candida present — at a healthy level — before taking antibiotics are at a higher risk of a post-antibiotic yeast infection as well.
Estrogen levels
The sex hormone estrogen can play a role in the development of a yeast infection. This is why they are more common during pregnancy, when estrogen levels are raised, and in people who take hormonal contraception.
Weakened immune system
People with a weakened immune system, for example, those with HIV, are more susceptible to Candida overgrowth.
Uncontrolled diabetes
Yeast feeds off sugar, so uncontrolled blood sugars can encourage yeast to overgrow.
Chemicals and fragrances
When used to clean the vagina, irritants such as perfumed soaps, shower gels, and feminine hygiene products can alter the vagina’s natural pH, creating favorable conditions for yeast overgrowth.
Remember, you also don't need to clean out your vagina with any sort of liquid or gel — it's self-cleaning!
Tight clothing
Synthetic and poorly-ventilated clothing are also thought to increase the risk of infection, as this can increase the temperature and moisture levels around the perineal area — between the anus and the vulva — and cause Candida to overgrow. However, more research is needed here. In the meantime, the Centers for Disease Control and Prevention (CDC) suggests wearing cotton underwear.
Sex
A yeast infection isn’t considered a sexually transmitted infection, but sometimes sexual activity can create conditions that encourage Candida to overgrow.
Get care for vaginal yeast infections with Evvy
We've created the first-ever platform for vaginal healthcare that combines state-of-the-art vaginal microbiome testing, prescription treatment, and 1:1 coaching to get you the answers, relief, and support that you deserve.
Built with leading OB-GYNs and researchers, Evvy's care platform can connect you to providers trained to review your vaginal microbiome results and select the best antifungal to decrease your specific strains of Candida (including ones that aren't often tested for at the doctor's office.)
They'll also recommend research-backed supplements to build back your microbiome to a protective state. Experience vaginal health care with Evvy today.
FAQ
What usually causes a yeast infection?
Yeast infections are caused by an overgrowth of Candida fungi, typically Candida albicans. Candida can overgrow when the natural balance of microorganisms in the vagina is thrown off. Risk factors for yeast infections include hormonal changes from pregnancy or birth control, a weak immune system, poorly controlled diabetes, high estrogen levels, wearing tight or non-breathable clothing, and using douches or scented vaginal products.
How do you know if you have a yeast infection?
You may have a yeast infection if you're experiencing symptoms like itching, irritation, and swelling in the vaginal area, along with a thick, white discharge resembling cottage cheese. To be certain, it's best to see a healthcare provider who can perform a pelvic exam and take a sample of the vaginal discharge to examine under a microscope or in a lab. If you're experiencing symptoms of a yeast infection, you can also consider taking an Evvy vaginal microbiome test for peace of mind. It's important to remember that similar symptoms can indicate other conditions, so seeking professional advice is the best way to ensure accurate diagnosis and treatment.
Can men get yeast infections?
Men can also get yeast infections from sex! It’s estimated that around 15% of people with a penis who have unprotected penetrative sex with someone with a yeast infection go on to develop a penile yeast infection.