

Is a Bladder Infection the Same as a UTI? Understanding the Difference
Learn whether a bladder infection is the same as a UTI, key differences, and how Evvy’s UTI+ Test helps uncover root causes and effective treatment.
Words by Olivia Cassano
Scientifically edited by Dr. Krystal Thomas-White, PhD
Medically reviewed by Dr. Kate McLean MD, MPH, FACOG
If you’ve ever felt burning when you pee or suddenly needed to sprint to the bathroom, you might have immediately thought of a urinary tract infection (UTI). A UTI is any infection that occurs in the urinary tract — the system that includes your urethra, bladder, ureters, and kidneys. Because these structures are all connected, bacteria can enter the urethra and move upward, causing infection in different parts of the urinary system.
This leads to a very common question: Is a bladder infection the same as a UTI? The short answer is that a bladder infection is one type of UTI, but the term “UTI” is an umbrella term for all bacterial infections that affect the urinary system. UTIs can also occur in the kidneys or the urethra, each with different levels of severity.
Keep reading to learn the difference between a bladder infection and a UTI, why the terms often get confused, and how symptoms, treatment, and diagnostic approaches shift depending on the type of infection you’re dealing with.
The difference between a bladder infection and a urinary tract infection
A bladder infection is specifically a bacterial infection of the bladder that causes inflammation, and in medical terms, this is known as cystitis. It’s the most common type of UTI, and for many people, it’s their only experience with urinary infections. But the urinary tract is a whole interconnected system, and bacteria can infect different parts of it.
To understand the difference, it helps to picture the urinary tract's anatomy. Urine begins in the kidneys, where waste is filtered out of your blood. From there, thin tubes called the ureters carry urine into the bladder, which serves as a storage container. When you pee, urine exits through the urethra, a narrow passage that leads outside the body. The upper urinary tract includes the kidneys and ureters, while the lower tract includes the bladder and urethra. Each of these structures can technically develop an infection.
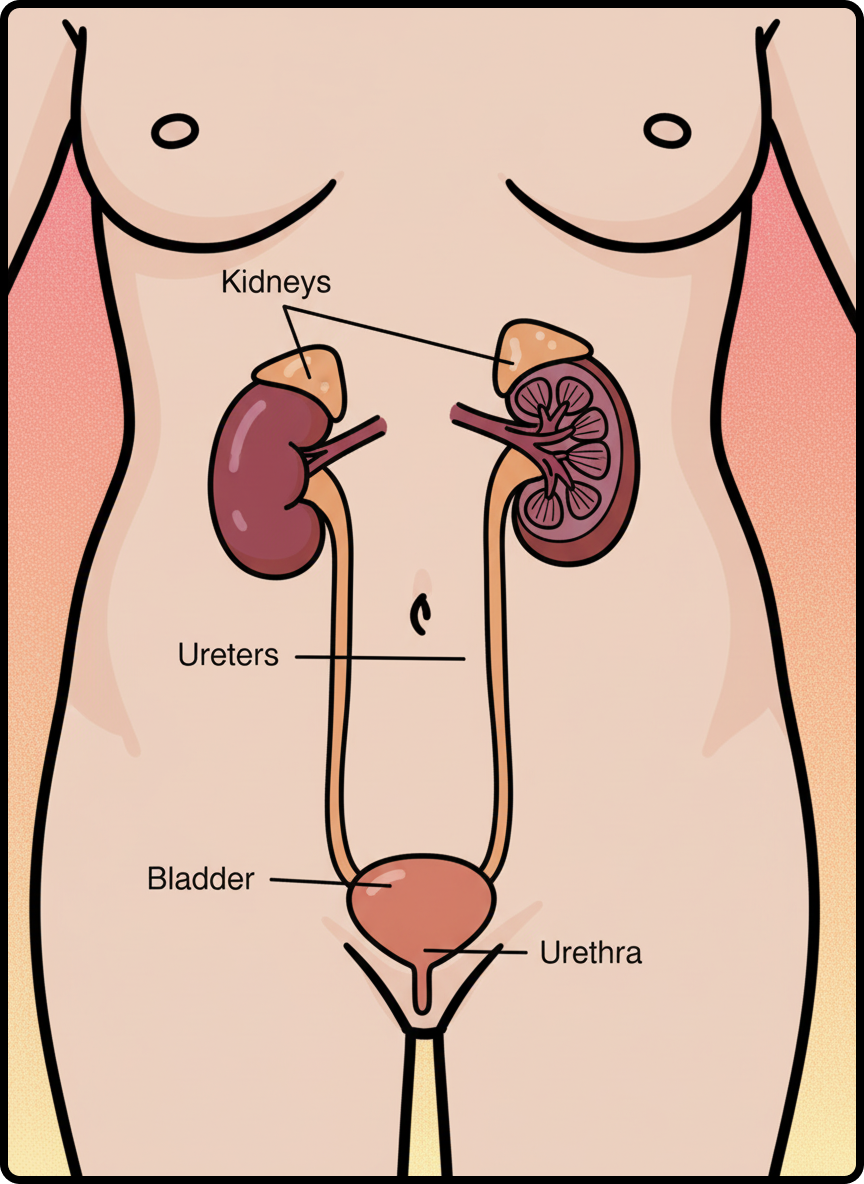
When clinicians say UTI, they’re referring to any infection that occurs anywhere in this system (upper or lower). Cystitis is considered a lower urinary tract infection because it’s localized to the bladder. An upper urinary tract infection, such as pyelonephritis, affects the kidneys and tends to be more serious.
A woman's urethra is shorter than a man's, which makes it easier for harmful bacteria (often from the vagina or gut) to travel upward and cause infection. Most of the time, the bacteria stop in the bladder. But if they continue upward, the infection becomes more severe. So, while every bladder infection is a UTI, not every UTI is a bladder infection.
Anatomy and terminology simplified
The urinary system can feel a little abstract, especially if your main interaction with it is simply the daily need to pee. But understanding the basic layout helps clarify why infections behave the way they do.
Think of your kidneys as two efficient filters at the top of the system. They continuously draw waste from your bloodstream and produce urine. The ureters are like narrow slides delivering the urine downward into the bladder. The bladder itself is the reservoir: a flexible, muscular organ designed to stretch and hold urine until it’s convenient to release it. The urethra is the exit channel.
Cystitis refers specifically to inflammation or infection of the bladder, urethritis involves the urethra, and pyelonephritis affects the kidneys. The term UTI can refer to any of these conditions. The specificity of healthcare providers' terminology depends on factors such as your symptoms, the severity of those symptoms, clinical findings, and your treatment needs.
Why the terms are often used interchangeably
Most people use “UTI” to refer to any infection that causes discomfort when you pee or have urinary urgency. Since the majority of UTIs are bladder infections, it’s easy to see why the distinction has blurred.
In practice, the most common UTI symptoms start similarly, regardless of where the infection is. That means many people don’t know where their infection is located until more severe symptoms appear or until a clinician performs specific tests. And because treatment for most uncomplicated bladder infections is relatively consistent, people naturally refer to all urinary discomfort as “a UTI.”
However, the interchangeable use of these terms can sometimes lead to confusion, particularly for people who experience recurring infections. Understanding exactly what kind you have — and whether the infection has moved beyond the bladder — is the best way to make sure you’re getting the right care and solving the root of the issue if UTIs keep coming back.

Recurrent symptoms? Get Evvy's at-home vaginal microbiome test, designed by leading OB-GYNs.
Comparing symptoms, treatment, and severity
At first glance, cystitis and a broader urinary tract infection can look almost identical. Both may start with a burning feeling when you pee, pelvic discomfort, and that unmistakable feeling of needing to pee every few minutes. But the key difference is what happens next. When an infection stays confined to the bladder, the symptoms tend to be uncomfortable but manageable. When the infection spreads to the kidneys, symptoms typically develop into something more serious.
- A lower urinary tract infection, which includes cystitis, generally causes localized discomfort. You may feel a sharp burn when you pee, notice cloudy or strong-smelling urine, or feel constant pressure in your crotch. Many people describe the sensation as having to pee all the time, even immediately after going.
- An upper urinary tract infection, which affects the kidneys, tends to cause systemic symptoms. Instead of being limited to the bladder area, the infection starts to affect your whole body. Fever is common, as are chills, nausea, or vomiting. You might feel a deep ache or throbbing in your lower back or along your sides, known as flank pain. These symptoms indicate that the infection is no longer localized and is now something that requires prompt medical attention.
Treatment also differs based on severity. Mild bladder infections are often treated with a short course of antibiotics, though growing antibiotic resistance means treatment isn’t always one-size-fits-all. Kidney infections, on the other hand, often require stronger or longer antibiotic courses, and in severe cases, intravenous antibiotics or hospitalization.
Common bladder infection symptoms
Cystitis almost always starts with a familiar combination of urinary symptoms:
- A sharp, burning sensation when you pee
- A frequent need to pee
- Feeling like you can’t fully empty your bladder
- Cloudy, strong-smelling urine
- A feeling of pressure that doesn’t quite go away.
In elderly women, urinary incontinence is often the only symptom they show.
When it becomes more than a bladder infection
Cystitis becomes a more serious infection when it's left untreated, and bacteria travel upward from the bladder to the kidneys. This shift can happen gradually or quite suddenly, and the symptoms often make the change crystal clear.
The telltale signs include fever, chills, nausea, or vomiting. Many people also experience pain in their back or sides, which may feel like a deep ache or a sharp, stabbing sensation.
A kidney infection is considered a serious medical concern because the kidneys are critical organs that filter waste from your blood. When an infection reaches them, it can lead to severe complications such as sepsis (an infection of the bloodstream) if not treated in time.
How diagnostic approaches differ between a single infection and recurrent UTIs
When you're experiencing your first bladder infection (or even if you just face one every so often), the process to figure things out is usually pretty straightforward. Doctors typically start by looking at your symptoms and doing a simple urine test to check for the presence of bacteria or signs of inflammation.
However, if you find yourself dealing with urinary tract infections over and over again, the approach changes a bit. Recurrent urinary tract infections can indicate that something else might be going on that’s contributing to these frequent infections. This could be anything from stubborn bacteria to antibiotic resistance, anatomical factors, or even certain habits. Because of this, doctors generally take a more detailed look to understand what's really happening.
When it comes to recurrent UTIs, urine cultures are often needed to pinpoint the specific bacteria involved, along with bacterial antibiotic susceptibility testing to see which antibiotics can effectively tackle them. Sometimes, they might recommend imaging studies like ultrasounds to check for any structural issues, like kidney stones or blockages. Additionally, doctors may consider factors such as hormonal changes, imbalances in vaginal microbiomes, or ongoing inflammation that could make someone more susceptible to infections.
This layered approach ensures that treatment targets the underlying cause rather than just the repeated symptoms.
Evvy’s UTI+ Test offers even deeper insights by identifying bacterial strains and antibiotic resistance markers that traditional tests might miss. For people who experience frequent bladder infections, these more advanced diagnostics can make the difference between short-term relief and long-term solutions.
Standard testing for a single bladder infection
When you have cystitis for the first time, doctors usually start by looking at your symptoms and performing simple urine tests. A routine urinalysis usually includes a dipstick test and a microscopic test. The dipstick test checks your urine for signs of inflammation, like pH, white blood cells, red blood cells, nitrites, and leukocyte esterase. A microscopic test will take a quick look at your urine under a microscope and human and bacterial cells.
Since bladder infection symptoms are often obvious, many doctors feel confident diagnosing a simple bladder infection just by hearing about your symptoms, especially if they match common signs and there are no serious warning signs. After that, they may give you antibiotics and watch how you respond to the treatment.
Diagnostic workup for recurrent UTIs
Frequent UTIs need a careful check. Doctors don’t just rely on your symptoms or simple urine tests. They usually order urine cultures. This test grows the bacteria in your urine and identifies the specific types causing your infection. After identifying the bacteria, they also test which antibiotics will work best.
Doctors might recommend imaging tests, like an ultrasound of the kidneys or bladder, to look for any physical problems that could cause ongoing infections. Depending on your situation, they may also check how well your bladder empties or look for urinary stones.
This is where Evvy’s UTI+ Test can help. Unlike regular urine cultures that only find certain bacteria, Evvy’s test uses advanced technology to identify the germs responsible, even those hard to detect with standard methods. It also shows any antibiotic resistance that might be causing recurring infections. This detailed information helps doctors create a more tailored and effective treatment plan, especially for those who keep experiencing UTIs.
Preventing recurrence and supporting urinary health
Preventing UTIs isn’t always simple, especially if you’re someone who seems to get them often. But there are proactive steps that can make a meaningful difference:
- Stay well-hydrated. Drinking enough water helps keep your urine dilute and naturally flushes bacteria out of your urinary system before they have the chance to multiply.
- Know that female anatomy matters. People assigned female at birth have a shorter urethra, allowing bacteria a shorter distance to travel to reach the bladder, making UTIs more common.
- Always complete your antibiotic course. Even if you start feeling better early, stopping antibiotics too soon can allow lingering bacteria to regrow and potentially become resistant.
- Pee after sex. Sexual activity is a common UTI trigger, and urinating afterward can help clear bacteria from the urethra.
- Keep hygiene gentle. Harsh soaps, douches, or over-cleansing can irritate the vulva and disrupt your natural microbiome, leaving you more prone to infection. Gentle washing with water or mild products is usually more protective.
- Consider hormonal shifts. During perimenopause and menopause, lower estrogen levels can change the vaginal and urinary tissues, increasing susceptibility to UTIs. In some cases, vaginal estrogen (if recommended by your healthcare provider) may help.
- Identify deeper causes of recurrence. Frequent infections may stem from chronic inflammation, persistent bacteria, pelvic floor issues, or microbiome imbalances. Evvy’s UTI+ Test can help uncover underlying contributors by showing which microbes are present and how they may be driving repeated infections.
When to talk to your clinician about bladder or urinary tract infections
It's really important to know when to seek medical care, especially with bladder infections. If you’re experiencing mild symptoms for the first time, it’s a good idea to reach out to your healthcare provider. Getting treatment early can help prevent things from getting worse. However, if your symptoms start to escalate — like developing a fever, back pain, or nausea — or just feel different from what you’re used to, don’t hesitate to seek care right away.
If you've started antibiotics and your symptoms stick around, give your doctor a call. Sometimes, the bacteria can be resistant to the medication, and a change in treatment might be needed. Also, if you find yourself dealing with multiple UTIs a year, it’s definitely worth having a chat about a more thorough evaluation. Recurrent infections can sometimes point to an underlying issue that needs attention.
Taking the next step with Evvy
If UTIs have become a recurring part of your life, you deserve more than quick fixes. You deserve clarity and fast, accurate answers you can trust. UTIs are the most common infection in the U.S. for women, with half of all women experiencing at least one in their lifetime. Yet the standard testing methods we rely on are surprisingly limited. Traditional urine cultures can miss up to 50% of pathogens and often take days to return results. In the meantime, you’re left waiting, wondering, and hoping your symptoms don’t get worse.
It’s no surprise that many people end up with treatments that miss the mark. Nearly one in two women is prescribed an antibiotic that may not actually work against their infection, and three in four receive longer courses of antibiotics than necessary. This trial-and-error cycle isn’t just frustrating; it can prolong symptoms and contribute to antibiotic resistance. When you’re dealing with pain, urgency, and disruption to your daily life, you need the right treatment the first time.
Instead of relying on guesswork, Evvy’s UTI+ Test uses PCR technology to detect pathogens that standard cultures frequently miss, delivering results within one business day of arrival at the lab. The test identifies the exact bacteria causing your symptoms and the antibiotic resistance genes that may make certain treatments ineffective. That means your provider can prescribe the medication that will actually work.
And if UTIs keep coming back, Evvy can help uncover the deeper “why.” About one in four women experiences recurring UTIs, and research shows that bacteria from the vaginal microbiome can migrate to the bladder and trigger repeat infections. In fact, among Evvy users who reported a recent UTI, 47% had UTI-related bacteria present in their vaginal microbiome — an overlooked contributor to recurrence. Evvy’s UTI+ Test examines this connection, giving you and your clinician insight into whether your vaginal microbiome is part of the cycle.
On top of accurate testing, you can support your urinary tract health with Evvy Women’s Complete Probiotic. Our 3-in-1 formula is designed to support the vaginal, gut, and urinary microbiomes — three ecosystems that are closely connected when it comes to UTI risk. By helping replenish good bacteria and maintain a balanced vaginal environment, this probiotic may reduce the chances of harmful bacteria moving from the vagina to the bladder, which is a common pathway for recurrent UTIs. A healthier vaginal microbiome can mean stronger natural defense against the bacteria that often trigger UTIs.
Instead of reacting to symptoms over and over, you gain the ability to prevent infections at the source. With Evvy, you get data-backed insights, targeted treatment, and a clearer path toward long-term urinary health.
FAQs about bladder infections and UTIs
How do you confirm a bladder infection or UTI?
A bladder infection or UTI is usually confirmed through a urinalysis, which looks for markers of inflammation or bacteria. For more detailed information, a urine culture may be done to identify the specific bacteria responsible and determine which antibiotics are likely to work. In recurrent cases, additional testing may be recommended to uncover underlying causes.
Can UTIs cause vomiting?
Yes. Vomiting is more commonly associated with kidney infections rather than uncomplicated bladder infections. If you’re experiencing nausea, vomiting, fever, or flank pain, this may be a sign that the infection has spread beyond the bladder and requires prompt medical attention.
What are the warning signs of a bladder infection?
The most common early signs include burning during urination, urinary urgency, frequent urination, pelvic pressure, and cloudy or strong-smelling urine. If these symptoms are accompanied by fever, back pain, or nausea, it may be more than a bladder infection and should be evaluated quickly.





.avif)