
Trichomoniasis vs BV: How to Tell the Difference
Compare BV vs trichomoniasis by discharge, odor, symptoms, and testing methods, and learn about co-infections and treatment options.
Words by Olivia Cassano
Scientifically edited by Dr. Krystal Thomas-White, PhD
Medically reviewed by Dr. Kate Stewart, MD
When it comes to vaginal health, it's important to understand the differences between common infections for effective treatment and overall well-being. Two conditions that often cause confusion due to their similar symptoms are trichomoniasis and bacterial vaginosis (BV).
Both can lead to discomfort and long-term complications to your reproductive health if left untreated, but they differ significantly in their causes, transmission, and treatment methods.
Below, will delve into the specifics of trichomoniasis vs BV, highlighting their key differences to help you identify and manage these conditions more effectively.
What is BV?
Bacterial vaginosis is a vaginal infection caused by the overgrowth of harmful bacteria in your vaginal microbiome, most commonly, Gardnerella and Prevotella.
Bacterial vaginosis is the most common vaginal condition in women ages 15-44, and almost 30% of people with vaginas get bacterial vaginosis each year, according to the Centers for Disease Control (CDC).
BV occurs when the harmful bacteria in your vaginal microbiome grow faster than the protective bacteria (lactobacilli), resulting in an imbalance of naturally occurring bacteria called dysbiosis.
Research shows that certain activities or events put you at an increased risk of BV, including:
- Unprotected sex (especially with multiple sexual partners or a new sex partner)
- Hormonal fluctuations (e.g., birth control, pregnancy, and menopause)
- Your period
- Smoking
- Stress
- Douching and using feminine hygiene products.
Is BV a sexually transmitted infection?
No, bacterial vaginosis isn't a sexually transmitted infection (STI), and anyone with a vagina can get bacterial vaginosis (even if they’re not sexually active), but certain sexual behaviors can trigger BV. Having unprotected sex or having multiple sex partners are risk factors for BV.
Although it’s not a sexually transmitted infection, having bacterial vaginosis can increase your risk of contracting an STD.
How to know if you have BV
There are two diagnostic methods to know if you have bacterial vaginosis: by looking at your symptoms or with a swab test.
The symptomatic diagnosis uses the Amstel criteria, which require you to have three out of four symptoms, which your medical provider will evaluate for:
- thin, gray/white discharge
- clue cells
- a vaginal pH over 4.5
- a fishy odor.

Recurrent symptoms? Get Evvy's at-home vaginal microbiome test, designed by leading OB-GYNs.
The safest bet is to see your healthcare provider rather than self-diagnosing. Research shows that most of us aren't very good at self-diagnosing bacterial vaginosis.
One study showed that only 56% of self-diagnoses of bacterial vaginosis were correct. It’s also worth remembering that bacterial vaginosis doesn’t always cause symptoms, so you can’t rely on those alone.
The second way to diagnose bacterial vaginosis is by using the Nugent score diagnosis, which involves examining a vaginal smear under a microscope and counting three bacterial morphotypes — Lactobacillus, Gardnerella, and curved gram rods. A score under 4 is healthy, 4-7 is intermediate, and 7-10 is BV.
Whether or not you're dealing with symptoms, Evvy's at-home vaginal microbiome test screens for any infection-causing fungi and bacteria, including ones linked to BV.
What is trichomoniasis?
Trichomoniasis, or “trich,” is one of the most common non-viral sexually transmitted infections in the US. Anyone sexually active can get it, but women have an increased risk of contracting trich because the parasite that causes it tends to thrive in moist environments like the urethra, vagina, and vulva.
Trichomoniasis is caused by a parasite called Trichomonas vaginalis (TV). It's spread through unprotected sexual contact and bodily fluids such as semen and vaginal fluid.
You can get tested for trichomoniasis at your healthcare provider's office or a sexual health clinic. The test is known as NAAT (nucleic acid amplification tests).
During the test, your healthcare provider will do a pelvic exam and take a sample with a vaginal swab, which will be sent to a lab for testing.
Trichomoniasis tests aren't always included in routine STI panels, so you might need to ask for it specifically. You can also do an at-home test for trichomoniasis with Evvy's Expanded PCR Panel and Vaginal Health Test. All you have to do is take the sample yourself and send it to a lab for analysis.
Even if you don't have any trich symptoms, it's a good idea to make testing a regular part of your STI screening routine.
Can you have BV and trichomoniasis at the same time?
Yes, you can have BV and trichomoniasis at the same time, and it’s actually pretty common. Studies have found that a large number of women with trichomoniasis also have BV, with some research showing co-infection rates as high as 60–80%.
The CDC points out that having BV can make it easier to get trichomoniasis, and the two often show up together. When both infections are present, it’s important to treat them properly, because they can raise the risk of HIV and lead to other health problems, especially during pregnancy.
Since treatment for BV and trichomoniasis isn’t always the same, doctors often check for both if one is found. Catching and treating both help protect your health and prevent complications.
Symptoms comparison: BV vs trichomoniasis
Although they’re very different infections, BV and trich share a lot of similar symptoms — the most common symptom being foul-smelling discharge.
Bacterial vaginosis symptoms
The most common signs and symptoms of bacterial vaginosis are:
- a strong, unpleasant, or fishy vaginal odor that gets worse after sex
- abnormal vaginal discharge that is thin and watery and is usually white or gray
- In some cases, pain, itching, or a burning sensation in the vagina.
Bear in mind that bacterial vaginosis can be asymptomatic, and up to 84% of people with bacterial vaginosis may not experience anything at all.
Trichomoniasis symptoms
Some common trich symptoms include:
- Genital itching and irritation
- Abnormal vaginal discharge that is thin and frothy and is green or grey
- A foul or fishy odor
- A burning sensation when you pee
- The frequent need to pee
- Spotting or bleeding between periods
- Pain during sexual intercourse.
Similar to BV, trichomoniasis can often be asymptomatic. Around 70% of people with trichomoniasis don't experience any symptoms at all, according to the CDC.
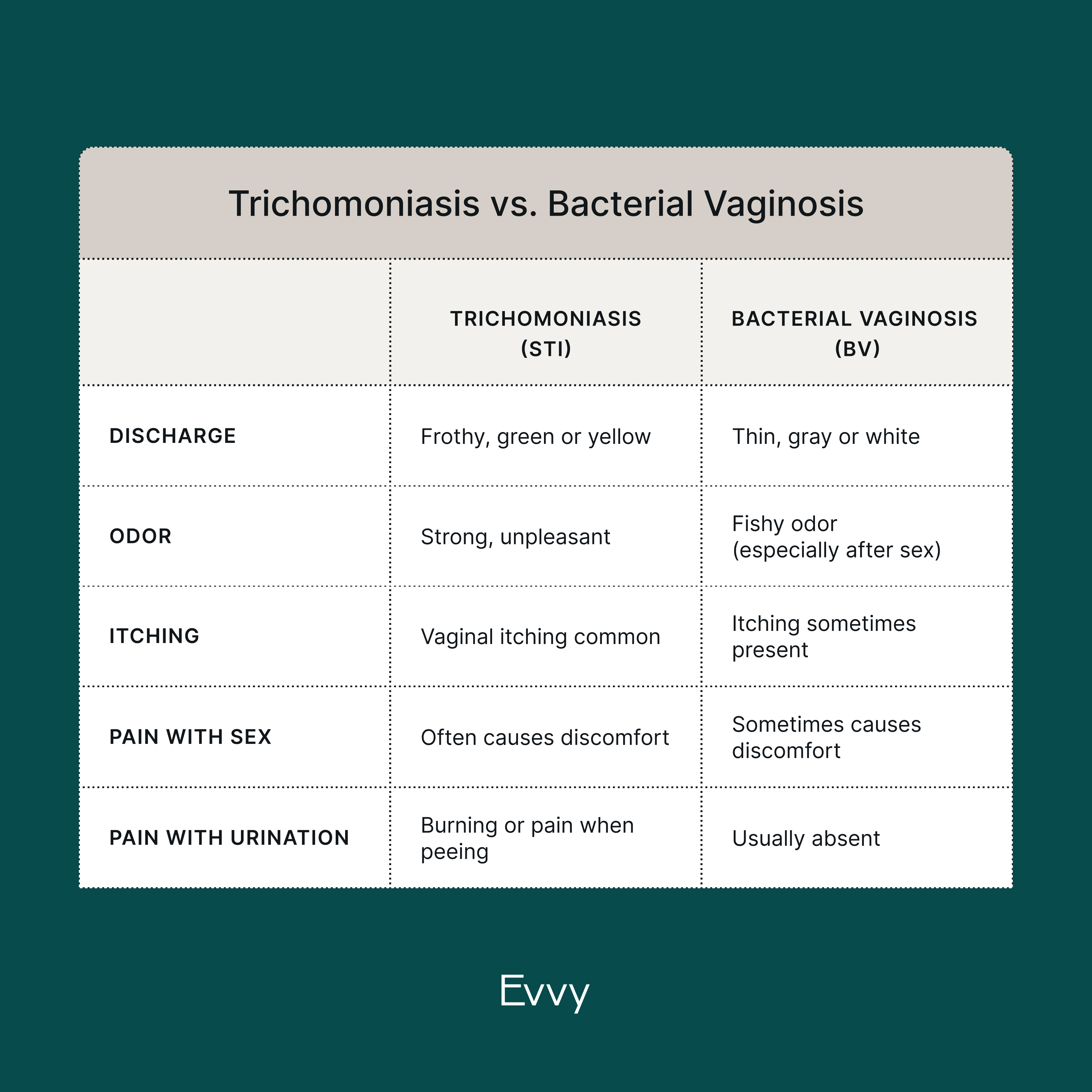
Discharge comparison: BV vs trichomoniasis
BV and trichomoniasis can cause similar symptoms, especially unusual vaginal discharge and vaginal odor. There are some slight differences between the two, though.
Trichomoniasis typically causes frothy, green discharge that has either a foul or fishy smell. Bacterial vaginosis is associated with watery, gray discharge with a fishy smell.
Other vaginal infections — including yeast infections and other STIs — can also cause changes in the way your discharge looks or smells. If you notice any unusual symptoms, it's a good idea to see your healthcare provider.
How to confirm BV vs trichomoniasis
The only way to know for sure if you have BV, trichomoniasis, or both is through testing. Healthcare providers often start with a vaginal pH test, followed by microscopy to look for clue cells (for BV) or motile parasites (for trichomoniasis). More accurate results come from nucleic acid amplification tests (NAATs), which detect the genetic material of Trichomonas vaginalis and BV-associated bacteria.
Evvy’s Vaginal Health Test offers a convenient at-home option. It uses advanced metagenomic sequencing to identify the full range of vaginal microbes, including those that cause BV and Trichomonas vaginalis. After you submit your sample, a licensed provider will review your results, confirm any diagnosis, and — if you’re eligible — prescribe treatment that can be delivered directly to your door.
How to treat trichomoniasis
Trichomoniasis is easily treatable with oral antibiotics. There are two common medications available: metronidazole and tinidazole. Metronidazole is usually given in a single dose, while tinidazole is taken in a lower dose twice a day for seven days.
One thing to keep in mind is that you should avoid alcohol during treatment. Also, you and your sex partner must receive treatment, even if your partner has no symptoms. People with penises don't usually experience symptoms, but they can still be infected and spread trich to others. So, getting treated as soon as possible is best to avoid spreading trichomoniasis to other partners.
BV treatment
Prescription antibiotics (metronidazole, clindamycin, tinidazole, etc.) are the first-line option for treating BV. They can either be taken orally or vaginally, depending on how bad your symptoms are.
Annoyingly, bacterial vaginosis has a nasty habit of returning even after treatment. While antibiotics clear up to 85% of BV cases within a month, over half of people experience a relapse within six months. Some studies have even shown recurrence rates as high as 80% even after what was considered "effective treatment" for three months.
Over-the-counter BV treatment
It can be extremely frustrating to have to take antibiotics repeatedly to treat BV. Unfortunately, no FDA-approved over-the-counter medicines for bacterial vaginosis are currently available.
Some research shows that boric acid vaginal suppositories might be a promising alternative, but we need more data to know for sure. In one study, a dual treatment for BV using boric acid and antibiotics kept 87% of patients symptom-free for 12 weeks after diagnosis. The positive results didn't last for everyone, though, and the patients still needed antibiotics in the first place. It's also important to note that healthcare professionals don't recommend using boric acid to treat BV.
Similarly, emerging research found that probiotic supplements could help prevent recurrent BV, but there still needs to be more evidence.
When it comes to vaginal infections, treatment should be personalized to your unique health history and vaginal microbiome, so it's really important to speak with your healthcare provider about potential over-the-counter solutions for BV. In the meantime, the Evvy vaginal microbiome test can help provide insights based on your microbiome to share with your medical provider.
FAQ
How to tell the difference between BV and trichomoniasis?
The only real way to tell the difference between bacterial vaginosis and trichomoniasis is to do an STI test. Bacterial vaginosis and trichomoniasis share a lot of symptoms, so it can be tricky to tell them apart. The main difference between BV and trichomoniasis is that BV occurs when there's an imbalance of normal bacteria in your vaginal microbiome, whereas trichomoniasis is a sexually transmitted infection caused by a tiny parasite that spreads through oral, vaginal, and anal sex. It's important to note that while trichomoniasis is a sexually transmitted infection, bacterial vaginosis isn't. However, sex is considered a risk factor for BV.
Can they mistake BV for trich?
It’s very easy to mistake bacterial vaginosis and a trich infection because they cause very similar symptoms — chiefly, unusual discharge with a fishy smell. Being misdiagnosed happens more often than being correctly diagnosed. In a study of 220 symptomatic patients, 61% of bacterial vaginosis diagnoses were incorrect. The best way to know whether you have bacterial vaginosis or trichomoniasis is to see your healthcare provider or take Evvy’s at-home vaginal health test, which screens for both bacterial vaginosis and trichomoniasis (and other sexually transmitted diseases).
Can BV and trich be treated at the same time?
It's possible to have a trich infection and bacterial vaginosis at the same time. The good news is that both of these can be treated with oral metronidazole therapy. Your healthcare provider may also prescribe a single oral dose of the antibiotic secnidazole, which research shows is effective in treating trichomoniasis in women with a bacterial vaginosis co-infection. This is currently the only FDA-approved single-dose treatment option for both of these common vaginal infections.
Do BV and trichomoniasis smell the same?
Both trichomoniasis and bacterial vaginosis can cause abnormal vaginal discharge with a strong or fishy smell. It’s normal for your vaginal discharge to have a mild smell (it comes out of your vagina, after all), but any drastic change in odor — especially if it’s foul or fishy — can be a warning sign of BV and trich, and warrants a trip to the OBGYN.
How do you confirm trichomoniasis or BV?
The only way to confirm trichomoniasis or BV is through testing. You can get tested at a healthcare provider’s office, sexual health clinic, or with Evvy’s at-home vaginal health test, which checks for BV-causing bacteria and Trichomonas vaginalis.





