

Probiotics for Menopause: Benefits, Bloating, and Vaginal Health
Discover how probiotics can support women during menopause, easing bloating, promoting vaginal health, and balancing gut and urinary microbiomes.
Words by Olivia Cassano
Scientifically edited by Dr. Krystal Thomas-White, PhD
Medically reviewed by Dr. Kate McLean MD, MPH, FACOG
Menopause can feel like a rollercoaster. Between changes in mood, sleep, digestion, and vaginal comfort, it’s a lot for your body to navigate. What many people don’t realize is that shifts in your gut and vaginal microbiomes play a big role in these symptoms. That’s where probiotics, or “good bacteria,” come in. By supporting balance in your body’s ecosystems, probiotics may help ease bloating, dryness, and other common changes during menopause. Keep reading to learn more about the link between menopause and these friendly bacteria, and the best probiotics for menopause symptoms.
What are probiotics and why do they matter in menopause?
Probiotics are live microorganisms (often bacteria and yeasts) that naturally live in your body. When present in the right balance, they help regulate digestion, immunity, metabolism, and even vaginal health. You can think of them as “friendly tenants” in your body’s microbiomes who help keep the peace.
During — and in the lead up to — menopause, your body experiences more than just hot flashes and mood shifts. A drop in estrogen also impacts the ecosystems of bacteria in your gut, vagina, and urinary tract. This matters because when microbial balance is disrupted, you may be more prone to symptoms like bloating, constipation, vaginal dryness and itching, or postmenopausal vaginal infections.
The “gut-vagina axis” describes the fascinating connection between these ecosystems. A disruption in the gut microbiome can affect the vaginal and urinary microbiomes, and that’s why addressing gut health with probiotics may ripple into improvements in vaginal comfort and urinary health (two key concerns during menopause).
Gut, vaginal, and urinary microbiomes
Your gut microbiome is the largest of the three, containing trillions of bacteria that help digest food, regulate blood sugar, and train your immune system. The vaginal microbiome is smaller but mighty — dominated by Lactobacillus species that maintain an acidic pH to keep harmful bacteria at bay. The urinary system has its own microbial defense system that helps prevent urinary tract infections (UTIs). Together, these three systems communicate with each other, influencing everything from hormone metabolism to inflammation.
Estrogen decline and microbial shifts in menopause
Estrogen plays a major role in vaginal health, chiefly by feeding Lactobacillus species in the vagina. These beneficial bacteria thrive on glycogen stored in vaginal cells, converting it into lactic acid that helps maintain an acidic pH and protects against harmful microbes.
Estrogen production slows down during perimenopause and menopause, leading to less glycogen and, in turn, fewer Lactobacillus. This reduction can have a big impact on the vaginal microbiome. Instead of being dominated by protective Lactobacillus, the vaginal environment becomes more diverse, with less protective anaerobic bacteria such as Prevotella, Gardnerella, and Fannyhessae/Atopobium taking hold. While increased microbial diversity might sound like a good thing (it usually is in the case of gut health), in this case, it actually signals a higher risk of dysbiosis and infection.
As Lactobacillus levels fall, vaginal pH rises, shifting from acidic to more neutral. This creates an environment where pathogens can flourish, increasing the likelihood of bacterial vaginosis (BV), yeast infections, and recurrent urinary tract infections. These microbial shifts are also linked to common genitourinary symptoms of menopause, including dryness, irritation, itching, and painful sex. Collectively, they contribute to urogenital atrophy, which can affect sexual well-being, urinary health, and overall quality of life.
Similarly, estrogen decline doesn’t just affect the vaginal microbiome. It can influence gut diversity, too. Some menopausal women experience a change in beneficial gut bacteria, which may contribute to constipation and bloating. Luckily, (the right) probiotics may help restore some of this lost balance by replenishing beneficial strains and supporting the gut, vaginal, and urinary ecosystems.

Recurrent symptoms? Get Evvy's at-home vaginal microbiome test, designed by leading OB-GYNs.
Benefits of probiotics for menopause
Probiotics are not a cure-all, but they may offer supportive relief for some menopausal symptoms. By positively influencing the gut and vaginal microbiomes, probiotics may reduce digestive discomfort, support vaginal health, and improve quality of life during this transition.
Bloating and digestion
Many menopausal women report new or worsening digestive issues (think gas, bloating, and irregularity). Probiotics can help by:
- Breaking down hard-to-digest foods like certain carbs and fibers.
- Producing short-chain fatty acids that support gut lining health and motility.
- Reducing gas-producing bacteria that contribute to bloating.
For example, strains like Lactobacillus plantarum may help to ease bloating, improve regularity, and decrease symptoms of irritable bowel syndrome (IBS).
Supporting vaginal pH and reducing dryness/itching
In the vaginal microbiome, Lactobacillus play a protective role by producing lactic acid, which maintains a slightly acidic environment. This acidic pH helps prevent vaginal infections while supporting vaginal comfort. Probiotics containing Lactobacillus strains may help restore a healthy vaginal flora and reduce symptoms like itching, dryness, and recurrent vaginal infections.
In addition, some probiotics can support urinary health by preventing harmful bacteria from taking hold in the urethra. That’s why certain formulations, like Evvy Women’s Complete Probiotic, are designed for vaginal and urinary tract wellness (along with gut health).
When used consistently, probiotics may provide daily support to ease bloating, support vaginal health, and improve urinary comfort during menopause.
What the research says about probiotics in menopause
Clinical research on probiotics in menopause is still developing, but the results so far are promising. Several randomized controlled trials have shown that probiotics can improve both physical and psychological symptoms of menopause in as little as six weeks.
- Symptom relief: Some studies reported improvements in Menopausal Rating Scale scores, which measure hot flashes, sleep quality, mood, and joint discomfort. While benefits are modest, they suggest that probiotics can help with overall well-being.
- Vaginal and urinary health: Other trials found probiotics improved vaginal health scores, lowered vaginal pH, and reduced inflammation. Women also reported fewer symptoms of dryness and irritation.
- Inflammation: Some probiotics lowered inflammatory markers, which is significant since menopause is linked to higher inflammation and risks of metabolic syndrome.
That said, the research isn’t perfect. Most studies are small, last only a few weeks, and test different probiotic strains at varying doses, which makes it hard to compare results. But while probiotics don’t match the effectiveness of hormone therapy for treating symptoms like hot flashes or vaginal atrophy, they’re a safe and gentle complement. Probiotics can help with issues like bloating, digestion, vaginal comfort, and urinary health, making them particularly appealing for menopausal women seeking non-hormonal alternatives. Therefore, while they’re not designed to substitute hormone replacement therapy (HRT), they can serve as a valuable addition to a comprehensive menopause management plan.
Who should consider probiotics during menopause?
While not everyone needs probiotics, certain women may benefit more than others, especially those dealing with microbiome disruptions.
Women with digestive issues or bloating
If constipation, irregularity, or uncomfortable bloating has become your new norm, probiotics can help restore gut balance and reduce digestive stress.
Frequent UTIs or vaginal discomfort
Because declining estrogen weakens vaginal defenses, probiotics may be especially helpful if you’re prone to vaginal dryness, irritation, or recurrent UTIs. Restoring Lactobacillus dominance can improve comfort and reduce the risk of both vaginal infections and urinary tract infections.
Post-antibiotic or recurrent infections
Antibiotics disrupt the microbiome by wiping out both harmful and beneficial bacteria. For menopausal women, this disruption can make symptoms worse. Probiotics can help repopulate beneficial strains and restore balance after antibiotic treatment.
How to choose the best probiotic for menopause
With shelves full of probiotic options, it can be overwhelming to know which one is right for menopause. The key is to look for strain variety, an appropriate Colony-Forming Unit (CFU) count, and a research-backed formula.
Strains that matter most
Strains with the most evidence for menopause-related symptoms include:
- Lactobacillus crispatus
- Lactobacillus rhamnosus
- Lactobacillus plantarum
- Lactobacillus acidophilus.
CFU counts and formulation differences
Many people assume more CFUs = better results, but that’s not always true. A product with 20 billion CFUs of irrelevant strains won’t be as effective as one with 5 billion CFUs of targeted, clinically backed strains. Delivery method also matters — capsules with delayed-release technology ensure the bacteria actually reach the intestines alive.
Probiotics + herbs: do they really work?
Some popular blends combine probiotics with herbs such as turmeric or moringa. While these herbs may have general health benefits, there’s limited clinical evidence supporting their role in relieving menopause-specific symptoms.
Evvy’s formula takes a different approach: focusing only on clinically studied probiotic strains for women’s gut, vaginal, and urinary health, avoiding unproven extras.
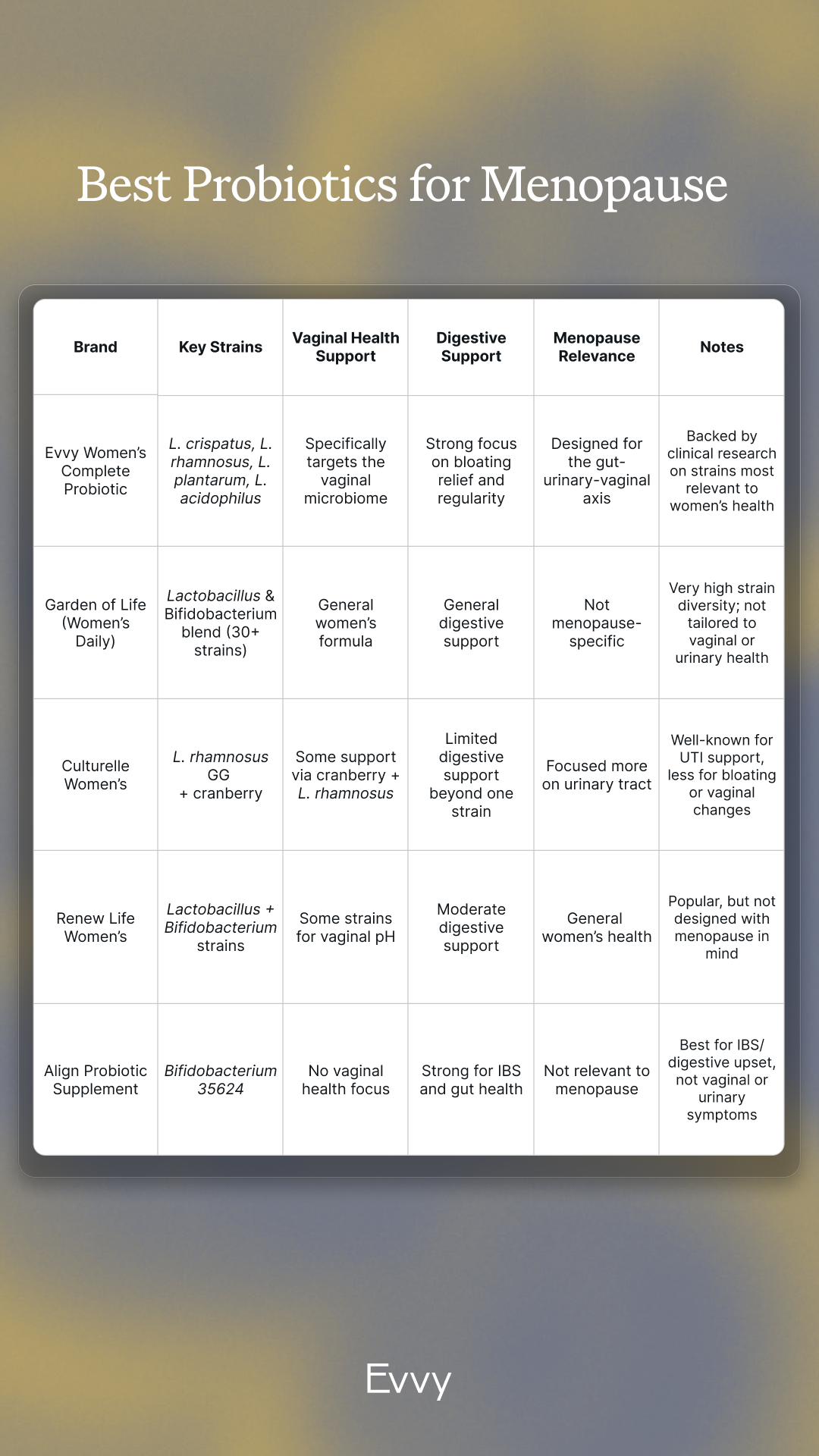
Best probiotics for menopause
When it comes to tackling bloating and vaginal discomfort, not all probiotics are equally effective. Evvy Women’s Complete Probiotic was formulated with the unique needs of women in mind, making it especially supportive during menopause. It includes clinically-studied strains such as Lactobacillus crispatus, L. rhamnosus, L. plantarum, and L. acidophilus — each chosen for their role in gut, urinary, and vaginal health — along with postbiotics and targeted vitamins for immune support.
This 3-in-1 approach acknowledges that these microbiomes don’t work in isolation, but in sync, influencing digestion, vaginal balance, and urinary comfort together. For menopausal women navigating microbial shifts, our formula helps promote healthy bacteria, support yeast balance, and reduce bloating with just one daily capsule.
How to use probiotics during menopause
Like all supplements, probiotics work best when taken consistently, not just occasionally.
Daily timing
Evvy Women’s Complete Probiotic should be taken once daily, either with food or on an empty stomach. It doesn’t really matter what time of day you take the capsule, as long as you’re consistent with it.
How long it takes to notice effects
In the first month of daily use, you may notice subtle gastrointestinal (GI) benefits, such as reduced bloating and more regular digestion, along with early improvements in vaginal health. Clinical trials on the strains included in Evvy Women’s Complete Probiotic indicate that by the third month of daily use, most people experience a stable vaginal pH and notice a reduction in vaginal odor and discharge as protective Lactobacillus populations increase. This is why we recommend using the probiotic for at least three months. Continuing daily use for up to six months further helps to reinforce and maintain a healthy microbiome across your gut, vaginal, and urinary tracts.
Safety and who should avoid probiotics
Probiotics are typically safe for healthy adults. However, if you are immunocompromised, pregnant, breastfeeding, taking medications (such as HRT), or have a medical condition, it is important to consult your healthcare provider before taking probiotics. If you experience ongoing digestive issues, it's advisable to consult a healthcare provider to rule out other potential causes.
How Evvy supports women in menopause
At Evvy, we recognize that menopause is a time of major change — not just hormonally, but also within the gut, vaginal, and urinary microbiomes. That’s why the Evvy Women’s Probiotic was formulated with strains shown to support bloating, digestion, and vaginal balance, areas that often shift during this transition.
In addition to our probiotic supplements, Evvy also offers Hyaluronic Acid Suppositories and a Soothing Vulva Cream, two options designed to address some of the most common and uncomfortable genitourinary symptoms of menopause. Vaginal dryness and painful sex often result from declining estrogen, which thins the vaginal tissues and reduces natural lubrication. Our Hyaluronic Acid Suppositories help replenish moisture and improve tissue hydration, while the Soothing Vulva Cream can calm irritation and support comfort in day-to-day life. Together, these non-hormonal options can provide relief for menopausal women looking to ease dryness and discomfort.
Evvy also offers a Vaginal Health Test that provides personalized insight into the state of your vaginal flora. Like vaginal health, menopause is incredibly subjective. Every woman’s experience is unique, and symptoms can vary widely in type, severity, and impact. That means treatment and management strategies shouldn’t be one-size-fits-all, but instead tailored to individual needs and preferences. Understanding your microbiome can be a valuable part of that process. An Evvy Vaginal Health Test offers insights into your unique microbial makeup, which can then be used alongside your healthcare provider’s guidance to design the right management protocol for you.
Paired with supportive tools like the Evvy Women’s Complete Probiotic or Vaginal Probiotic Suppositories, this approach recognizes that navigating menopause is highly personal — and that having information about your own body is an important step toward finding the strategies that work best for you.
FAQs about probiotics for menopause
What is the best probiotic for menopause?
The “best” probiotic supplement for menopause is one that supports the areas most affected by hormonal changes, namely digestion, vaginal health, and urinary balance. During menopause, estrogen decline can disrupt the vaginal flora, making women more vulnerable to dryness, irritation, and vaginal infections. At the same time, gut microbial diversity often shifts, which may contribute to bloating and constipation. Probiotics that contain strains like Lactobacillus crispatus, L. rhamnosus, L. plantarum, and L. acidophilus are especially helpful, as they are linked to restoring balance in both gut and vaginal ecosystems. Evvy Women’s Complete Probiotic was designed with this gut-urinary-vaginal connection in mind, making it highly relevant for menopause support. That said, the best choice for you may depend on your specific symptoms, health history, and goals, so it’s worth discussing options with your healthcare provider.
Do probiotics help with menopause belly fat?
Probiotics are not a weight-loss pill, and they won’t directly “melt away” menopause belly fat. However, there's some interesting evidence suggesting that our gut microbiome plays a role in how we manage metabolism, appetite, and inflammation — all factors that can influence weight gain during midlife. During menopause, hormonal shifts and changes in gut health can make it easier for abdominal fat to stick around. Probiotics can help support a healthy balance in your gut, reduce inflammation, and promote better digestion, which may make it easier to manage your weight. Some specific strains, like Bifidobacterium lactis, have even been studied for their potential benefits for metabolic health. While probiotics aren’t a substitute for a balanced diet, regular exercise, or hormone therapy if needed, they may be a nice addition to your overall strategy for managing menopause belly fat. Just keep in mind that their effects are usually modest, and more research is needed to draw definitive conclusions.
What do doctors prescribe for menopause?
Doctors often prescribe HRT, also known as menopausal hormone therapy (MHT), as the most effective treatment for significant menopausal symptoms, particularly hot flashes, night sweats, and moderate to severe vaginal dryness. HRT works by replenishing estrogen (and sometimes progesterone and testosterone), directly addressing the underlying causes of these symptoms. However, not all menopausal women are suitable candidates for HRT, and some may prefer non-hormonal alternatives. Probiotics aren’t considered a prescription treatment for menopause, but they can provide supportive benefits, particularly for digestive health, bloating, and vaginal comfort. Unlike HRT, probiotics don’t replace hormones; instead, they help restore the microbial balance that can be disrupted by a decline in estrogen levels. Many menopausal women choose to use probiotics in conjunction with or as an alternative to hormone therapy, based on their individual needs and preferences. Doctors may recommend incorporating probiotics into a comprehensive management plan for women seeking gentle, non-hormonal support.
Should a 50-year-old woman take probiotics?
For many women around age 50, probiotics can be a worthwhile addition to their wellness routine. At this stage of life, menopause or perimenopause often brings new challenges like bloating, digestive changes, recurrent UTIs, or vaginal dryness — all of which are linked to shifts in the microbiome. Probiotics may help by replenishing beneficial bacteria that support digestion, maintain a healthy vaginal pH, and bolster urinary tract defenses. While not every 50-year-old needs probiotics, they are generally safe for healthy adults and can provide support where imbalances arise. As with any supplement, it’s best to consult your healthcare provider, especially if you have chronic health conditions or take other medications.
What are the benefits of probiotics for menopause?
Probiotics offer several potential benefits during menopause, even though they aren’t a replacement for hormone therapy. First, they can support digestive health, helping reduce bloating, constipation, and irregularity, which often become more common in midlife. Second, they can help maintain vaginal health by replenishing protective Lactobacillus strains that decline with estrogen loss. This may reduce dryness, itching, discomfort, and the risk of vaginal infections. Third, probiotics may provide support for urinary health, as a balanced microbiome helps defend against recurrent UTIs. While probiotics won’t resolve severe hot flashes or night sweats, they can be a gentle, non-hormonal tool for easing some of the everyday discomforts of menopause.
Can probiotics help with menopause symptoms?
Yes, probiotics can help with certain menopausal symptoms, though their effects are usually modest. Research shows they may improve digestive discomfort like bloating and constipation, as well as genitourinary symptoms such as dryness, irritation, and postmenopausal vaginal infections. Some clinical trials have also reported improvements in overall menopausal symptom scores, including mild psychological symptoms, when women take probiotics consistently for several weeks. However, probiotics are not a substitute for hormone therapy, which remains the most effective treatment for menopausal symptoms. Instead, probiotics can be viewed as a supportive addition, especially for menopausal women who want non-hormonal options or who are focused on gut, vaginal, and urinary health. For many women, combining probiotics with lifestyle changes, nutrition, and other therapies provides the best balance of relief and long-term support.





