
What is the Vaginal Microbiome?
The vaginal microbiome is the ecosystem of bacteria, fungi, and more that lives inside the vagina, and it plays a major role in your overall health.
Words by the Evvy Team
Scientifically edited by Dr. Krystal Thomas-White, PhD
Medically reviewed by Dr. Sabrina Sahni, MD NCMP
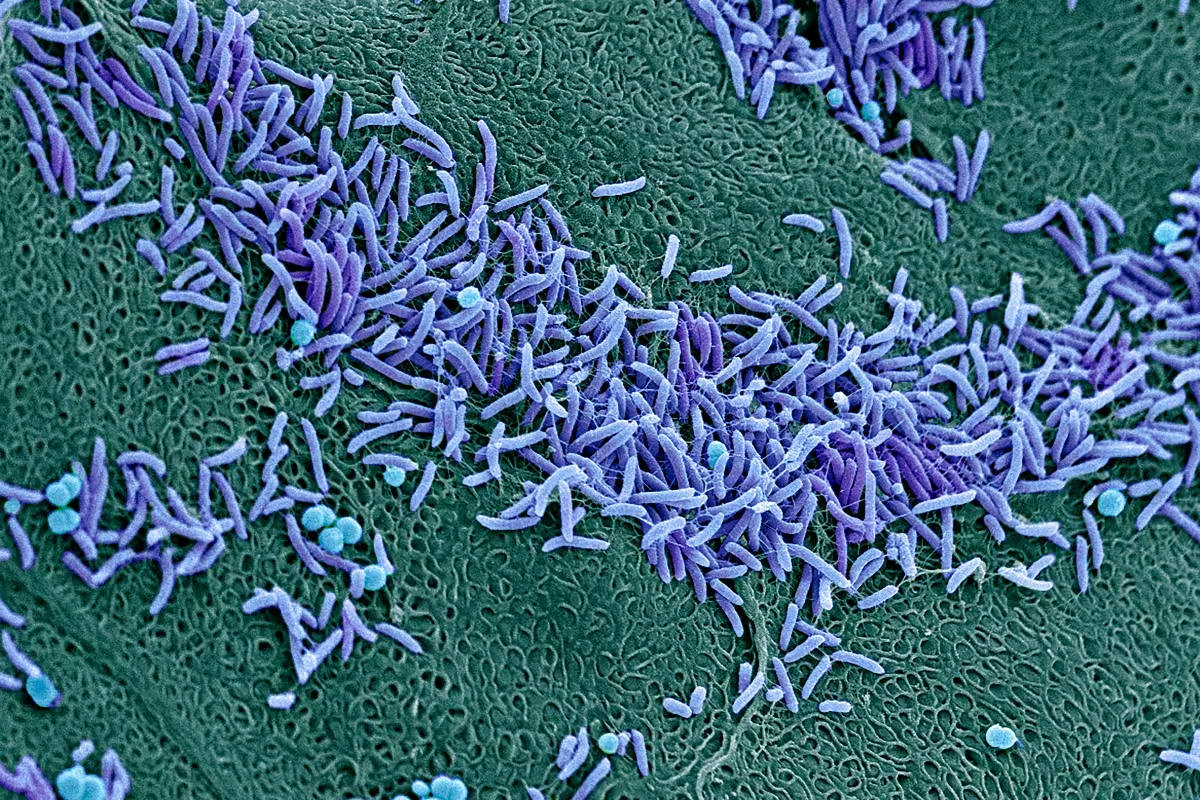
The vaginal microbiome is the complex ecosystem of microorganisms, including bacteria and fungi, that live inside the vagina (aka the vaginal microbiota or vaginal flora). Although you may have never heard of the vaginal microbiome, it plays a major role in your reproductive — and overall — health.
Vaginal discomfort is one of the leading reasons women seek healthcare advice, and over 90% of these cases can be attributed to imbalances in the vaginal microbiome. Imbalances in the vaginal microbiome can manifest as yeast infections, bacterial vaginosis (BV), cytolytic vaginosis (CV), aerobic vaginitis (AV) and more.
But your vaginal microbiome affects far more than just your vaginal health. An imbalanced vaginal microbiome is also associated with infertility, pregnancy complications, sexually transmitted infections (STIs), and possibly even cancer. So, why is it still such a mystery?
.jpeg)
Microbiome research is a fascinating field that's evolving quickly. While scientists have been working on deciphering the microbiomes of different parts of our bodies (like our gut and skin) for decades, the vaginal microbiome hasn't been given as much attention as it deserves — you can blame the gender health gap for that. But that’s why we’re here!
Keep reading to learn more about the vaginal microbiome, how it works, and how it could affect your reproductive health.
How does the vaginal microbiome work?
Your vaginal flora is made up of many different species of bacteria, fungi, viruses, and more, but there is one species of bacteria that plays a critical role in its health: Lactobacillus bacteria or lactobacilli, often referred to as the “good” or “protective” bacteria.
Lactobacilli are the MVPs of the vaginal microbiome and play a crucial role in keeping your vagina safe and healthy. They do this in a few different ways:
- Lactobacilli produce lactic acid to maintain a low pH level (between 3.8 and 4.5), which helps protect your vagina microbiome against harmful pathogens.
- Lactobacilli take up space on the vaginal wall to prevent other harmful bacteria from sticking around.
- Lactobacilli produce bacteriocins (your body's natural antibiotic) to stop disruptive bacteria from growing.
- Lactobacilli can help reduce inflammation in your genital area.
When there aren't enough protective bacteria like lactobacilli in your vaginal microbiome, disruptive bacteria like Gardnerella, E.coli, and Mycoplasma can take over and cause vaginal dysbiosis. Vaginal dysbiosis is an umbrella term used to describe a state of imbalance in the vaginal microbiome.
Vaginal dysbiosis can cause infections like bacterial vaginosis, yeast infections, urinary tract infections (UTIs), and more, leading to unwanted symptoms like itching, burning, irritation, and unusual vaginal discharge.

Recurrent symptoms? Get Evvy's at-home vaginal microbiome test, designed by leading OB-GYNs.
Vaginal infections and the microbiome
The most common type of vaginal dysbiosis is an infection called bacterial vaginosis (BV), which is clinically defined as an overgrowth of disruptive bacteria in the vaginal microbiome. This often happens when lactobacilli are depleted and pathogenic bacteria start to overtake the microbiome.
One in three women will get bacterial vaginosis each year, and up to 84% of these cases are asymptomatic. BV disproportionately affects Black and Hispanic women, with disappointingly lacking research as to why (that's one of the many things Evvy's here to change!).
But BV isn’t the only infection of the vaginal microbiome — there are many other forms of vaginal dysbiosis, such as yeast infections, aerobic vaginitis (AV), and cytolytic vaginosis (CV), which can have frustrating — and confusingly similar — symptoms, such as itchiness, abnormal discharge, and burning.
If you're here because you're dealing with recurring vaginal infections, just know that you're not alone. Bacterial vaginosis is the most common cause of vaginal symptoms among women, and at any given time, 1 in 3 women are dealing with bacterial vaginosis. 1 in 3 women will have a UTI by the time they're 24, and half will experience one at some point. And that's not all — a whopping 75% of women will experience a yeast infection at least once in their lifetime.
Despite vaginal discomfort being one of the leading causes why women and people with vaginas seek healthcare in the US, misdiagnosis and recurrence rates are high (over 50% for both!)
That's why Evvy built the world’s first and only metagenomic vaginal microbiome test and personalized clinical care: so we can provide more accessible and effective care for anyone with a vagina. While we're at it, we are also (finally) doing the research to better understand and treat these conditions.
The impact of the vaginal microbiome on overall health
It turns out that composition of the vaginal microbiome doesn’t just affect vaginal infections and symptoms — it plays a crucial role in female health, and emerging research has uncovered some groundbreaking insights into how it affects our overall well-being (beyond the vagina).
Research has shown that having a disrupted vaginal microbiome can create a favorable environment for infectious microorganisms to enter, increase inflammation, and inhibit your immune response within the reproductive tract, affecting the rest of your reproductive organs.
When protective bacteria like lactobacilli dominate the vaginal microbiome, it can make it harder for disruptive microbes to thrive, keeping the immune barrier of your reproductive tract strong and healthy.
Research has shown that having a disrupted vs healthy vaginal microbiome is associated with differing outcomes across:
- Contracting STIs such as chlamydia, gonorrhea, trichomoniasis, herpes, HPV, and HIV
- Pelvic inflammatory disease (PID)
- Fertility issues or failed IVF cycles
- Pregnancy complications such as miscarriage, preterm birth, neonatal problems, and preeclampsia
- Gynecological cancers such as ovarian, cervical, or endometrial cancer
- Cervicitis (inflammation of the cervix)
- Toxic shock syndrome (TSS).
By learning the composition of your unique vaginal microbiome, you can uncover how to proactively support its protective function and take a proactive approach to your long-term health.
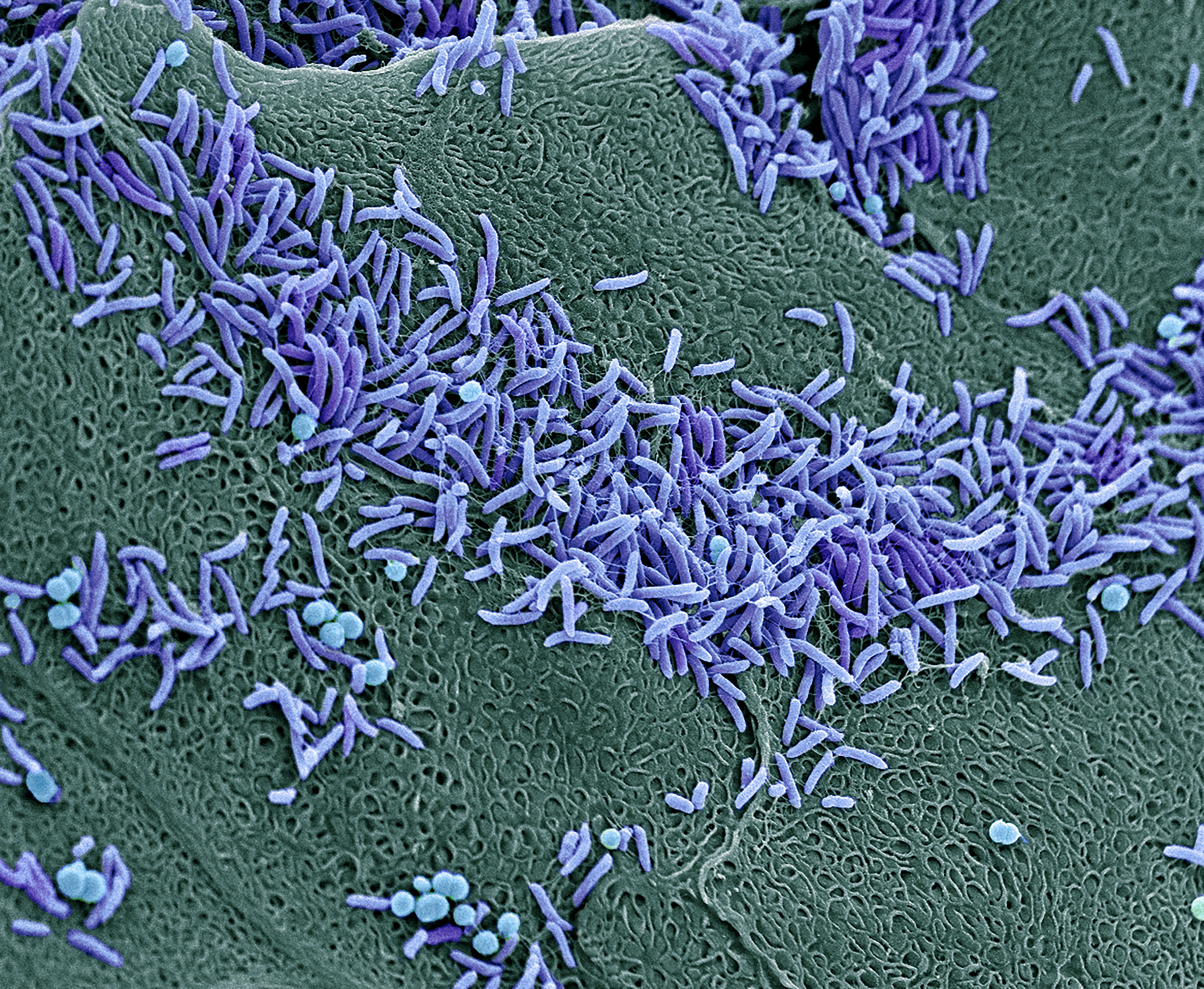
Does the vaginal microbiome change?
Your vaginal microbiome shifts with your behaviors, hormones, and more. There are many reasons that the vaginal microbiome can change, but some common ones include:
- Sex (especially new partners or multiple partners)
- Change in hormones e.g.
- Being pregnant or post-partum
- Going through menopause
- Changing birth control method
- Menstrual blood in the vagina
- Cyclical hormonal fluctuations
- Taking certain medications/supplements (especially antibiotics)
- Smoking
- Stress
- Using feminine hygiene products (especially douches)
.jpeg)
Not all vaginal microbiomes are the same
Just as there are different blood types, research has shown that most vaginal microbiomes fall into one of five general categories known as "Community State Types” (CSTs).
There are 5 general categories of CST, and the Community State Type is determined by which microbes are most dominant in your microbiome, and research has shown differences in symptoms, infections, and health outcomes across the CSTs. But the good news is that unlike blood types, you can switch from one CST to another as your microbiome shifts.
Of the five CSTs, four of them are dominated by a specific species of lactobacilli:
- Type 1: Lactobacillus crispatus
- Type 2: Lactobacillus gasseri
- Type 3: Lactobacillus iners
- Type 5: Lactobacillus jensenii
You're classified as Type 4 if you don't have a dominant species of lactobacilli. This group includes people experiencing vaginal infections but can also include some healthy vaginal microbiome compositions. That's why Type 4 is divided into five more subgroups. Want the deep dive? You can learn more in our comprehensive article on Community State Types.
.jpeg)
Want to know your vaginal microbiome CST?
With the Evvy vaginal microbiome test, you can find out all the bacteria and fungi in your microbiome and what CST your microbiome falls into at that moment. Although the research on these types is always improving, vaginal microbiome testing can provide insight into your individual microbial composition, both now and as it changes over time with your behaviors. Our team uses the most comprehensive data and advanced testing methods to help you understand what your type means for your health and what you can do to improve it.
FAQs
What does a vaginal microbiome test do?
A vaginal microbiome test is used to uncover the bacteria and fungi present in your vagina, which can contribute to symptoms like itching, odor, and discharge and infections like bacterial vaginosis (BV), yeast infections, UTIs and more.
We created Evvy’s at-home vaginal microbiome test to give you unique insights into your vaginal microbiome while raising awareness of the importance of research and clinical care for this often-overlooked part of the body.
Evvy’s vaginal microbiome test is the first-ever CLIA/CAP certified, metagenomic vaginal microbiome test to help you understand and improve your vaginal health. It’s a simple, at-home swab that uncovers all bacteria and fungi in your vaginal microbiome.
Testing your vaginal microbiome regularly can give you an idea of whether you're moving closer or farther away from an infection or disease. Your vaginal microbiome is constantly changing, and by catching any imbalances early on, you can help the good bacteria thrive and stop harmful bacteria from taking over.
And when you do change your routine — try a new probiotic, change your birth control, etc. — we'll take the guesswork out of figuring out how it’s affecting your microbiome. By testing your vaginal microbiome over time with an Evvy Membership, you can see how your life impacts your vaginal microbiome’s defense.





